LIMSwiki
Contents
| Eagle syndrome | |
|---|---|
| Other names | Styloid syndrome |
 | |
| Anteroposterior and lateral radiographs of cervical spine showing ossification of the stylohyoid ligament on both sides | |
Eagle syndrome (also termed stylohyoid syndrome,[1] styloid syndrome,[2] stylalgia,[3] styloid-stylohyoid syndrome,[2] or styloid–carotid artery syndrome)[4] is an uncommon condition commonly characterized but not limited to sudden, sharp nerve-like pain in the jaw bone and joint, back of the throat, and base of the tongue, triggered by swallowing, moving the jaw, or turning the neck.[1] First described by American otorhinolaryngologist Watt Weems Eagle in 1937,[5] the condition is caused by an elongated or misshapen styloid process (the slender, pointed piece of bone just below the ear) and/or calcification of the stylohyoid ligament, either of which interferes with the functioning of neighboring regions in the body, such as the glossopharyngeal nerve.[5]
Signs and symptoms
Possible symptoms include:
- Sharp, shooting pain in the jaw, back of the throat, base of the tongue,[1] ears, neck, and/or face[6]
- Difficulty swallowing[6]
- Sensation of having a foreign object in throat[6]
- Pain from chewing, swallowing, turning the neck, or touching the back of the throat[7]
- Ringing or buzzing in the ears
Classic Eagle syndrome is present on only one side; however, it may rarely be present on both sides.[6]
In vascular Eagle syndrome, the elongated styloid process comes in contact with the internal carotid artery below the skull. In these cases, turning the head can cause compression of the artery or a tear inside the blood vessel, which restricts blood flow and can potentially lead to a transient ischemic attack or stroke.[6] Sometimes, compression of the internal jugular vein can also occur and might lead to increased intracranial pressure.[8][9][10]
Cause
Eagle syndrome occurs due to elongation of the styloid process or calcification of the stylohyoid ligament, potentially compressing the nearby carotid artery or glossopharyngeal nerve.[5] However, the cause of the elongation hasn't been known clearly. It could occur spontaneously or could arise since birth. Usually normal stylohyoid process is 2.5–3 cm in length, if the length is longer than 3 cm, it is classified as an elongated stylohyoid process.[11] There are reports of eagles syndrome been elicited after wisdom tooth removal.[12]
Diagnosis
-
Radiograph, lateral view showing elongated stylohyoid process and stylohyoid ligament ossification
-
Radiograph, lateral view showing joint-like formation in ossified stylohyoid ligament
-
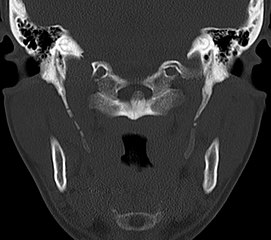
CT scan, coronal section showing bilateral extended styloid process and stylohyoid ligament ossification (incidental finding)
-
3D-reconstructed CT scan showing bilateral stylohyoid ligament ossification
-
3D reconstructed CT scan showing elongated styloid process (right side)
Diagnosis is suspected when a patient presents with the symptoms of the classic form of "Eagle syndrome" e.g. unilateral neck pain, sore throat or tinnitus. Sometimes the tip of the styloid process is palpable in the back of the throat. The diagnosis of the vascular type is more difficult and requires an expert opinion. One should have a high level of suspicion when neurological symptoms occur upon head rotation. Symptoms tend to be worsened on bimanual palpation of the styloid through the tonsillar bed. They may be relieved by infiltration of lidocaine into the tonsillar bed. Because of the proximity of several large vascular structures in this area this procedure should not be considered to be risk free.
Imaging is important and is diagnostic. Visualizing the styloid process on a CT scan with 3D reconstruction is the suggested imaging technique.[13] The enlarged styloid may be visible on an orthopantogram or a lateral soft tissue X ray of the neck.
Treatment
Treatment for Eagle Syndrome varies by case severity. Conservative methods typically include physiotherapy, long-acting anesthetics, and anti-inflammatory drugs.[14] More specifically NSAIDs, anticonvulsants, and antidepressants. NSAIDs are beneficial for inflammatory symptoms, while other medications target nerve-related pain.
Studies have shown that consistent physical therapy can significantly reduce pain and improve quality of life for patients with Eagle Syndrome.[14] Physical therapy aims to reduce overall pain by relaxing muscles around the calcified styloid ligament. Techniques may include manual therapy, stretching exercises, and specific movements to alleviate tension and improve muscle function.
Surgical Treatments
A partial styloidectomy is the preferred approach. Repair of a damaged carotid artery is essential in order to prevent further neurological complications.[citation needed] Regrowth of the stylohyoid process and relapse being a common occurrence is debatable.[7] Medical management may include the use of pain and anti-inflammatory medications, antidepressants, and/or corticosteroids. The overall success rate for treatment (medical or surgical) is about 80%.[15]
Epidemiology
Approximately 4% of the general population have an elongated styloid process, and of these about 4% give rise to the symptoms of Eagle syndrome.[5] Therefore, the incidence of stylohyoid syndrome may be about 0.16%.[5] More recent studies have reported the incidence of styloid elongation to be as high as 54%.[16]
Patients with this syndrome tend to be between 30 and 50 years of age but it has been recorded in teenagers and in patients > 75 years old. It is more common in women, with a male:female ratio ~ 1:2.[citation needed]
See also
References
- ^ a b c Waldman SD (6 June 2013). Atlas of Uncommon Pain Syndromes. Elsevier Health Sciences. pp. 35–36. ISBN 978-1-4557-0999-1.
- ^ a b Bumann A, Lotzmann U (2002). TMJ Disorders and Orofacial Pain: The Role of Dentistry in a Multidisciplinary Diagnostic Approach. Thieme. p. 279. ISBN 978-1-58890-111-8.
- ^ Taneja, Saumya; Chand, Sharad; Dhar, Shishir (March 2023). "Stylalgia and Styloidectomy: A Review". Journal of Maxillofacial and Oral Surgery. 22 (1): 60–66. doi:10.1007/s12663-022-01720-7. ISSN 0972-8279. PMC 9871118. PMID 36703673.
- ^ Hoffmann E, Räder C, Fuhrmann H, Maurer P (March 2013). "Styloid-carotid artery syndrome treated surgically with Piezosurgery: a case report and literature review". Journal of Cranio-Maxillo-Facial Surgery. 41 (2): 162–166. doi:10.1016/j.jcms.2012.07.004. PMID 22902881.
- ^ a b c d e Petrović B, Radak D, Kostić V, Covicković-Sternić N (2008). "[Styloid syndrome: a review of literature]". Srpski Arhiv Za Celokupno Lekarstvo. 136 (11–12): 667–674. doi:10.2298/sarh0812667p. PMID 19177834.
- ^ a b c d e Kamal A, Nazir R, Usman M, Salam BU, Sana F (November 2014). "Eagle syndrome; radiological evaluation and management". JPMA. The Journal of the Pakistan Medical Association. 64 (11): 1315–1317. PMID 25831655.
- ^ a b Sfcully C (21 July 2014). Scully's Medical Problems in Dentistry. Elsevier Health Sciences UK. ISBN 978-0-7020-5963-6.
- ^ Li M, Sun Y, Chan CC, Fan C, Ji X, Meng R (June 2019). "Internal jugular vein stenosis associated with elongated styloid process: five case reports and literature review". BMC Neurology. 19 (1): 112. doi:10.1186/s12883-019-1344-0. PMC 6549290. PMID 31164090.
- ^ Dashti SR, Nakaji P, Hu YC, Frei DF, Abla AA, Yao T, Fiorella D (March 2012). "Styloidogenic jugular venous compression syndrome: diagnosis and treatment: case report". Neurosurgery. 70 (3): E795–E799. doi:10.1227/NEU.0b013e3182333859. PMID 21866063.
- ^ Aydin E, Quliyev H, Cinar C, Bozkaya H, Oran I (2018). "Eagle Syndrome Presenting with Neurological Symptoms". Turkish Neurosurgery. 28 (2): 219–225. doi:10.5137/1019-5149.JTN.17905-16.6. PMID 27858390.
- ^ Raina D, Gothi R, Rajan S (2009). "Eagle syndrome". The Indian Journal of Radiology & Imaging. 19 (2): 107–108. doi:10.4103/0971-3026.50826. PMC 2765187. PMID 19881063.
- ^ Li S, Blatt N, Jacob J, Gupta N, Kumar Y, Smith S (August 2018). "Provoked Eagle syndrome after dental procedure: A review of the literature". The Neuroradiology Journal. 31 (4): 426–429. doi:10.1177/1971400917715881. PMC 6111425. PMID 28635381.
- ^ Karam C, Koussa S (December 2007). "[Eagle syndrome: the role of CT scan with 3D reconstructions]". Journal of Neuroradiology (in French). 34 (5): 344–345. doi:10.1016/j.neurad.2007.08.001. PMID 17997158.
- ^ a b Eagle Syndrome: Pathophysiology, Differential Diagnosis and Treatment Options, https://doi.org/10.52965/001c.67851
- ^ "Eagle syndrome". rarediseases. Genetic and rare diseases information center. Retrieved 17 April 2018.
- ^ Oztunç H, Evlice B, Tatli U, Evlice A (February 2014). "Cone-beam computed tomographic evaluation of styloid process: a retrospective study of 208 patients with orofacial pain". Head & Face Medicine. 10 (1): 5. doi:10.1186/1746-160X-10-5. PMC 3943457. PMID 24528515.