Infrastructure tools to support an effective radiation oncology learning health system
Contents
| Angina | |
|---|---|
| Other names | Stenocardia, angina pectoris |
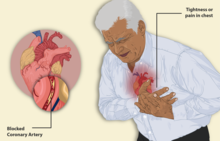 | |
| Illustration depicting angina | |
| Pronunciation | |
| Specialty | Cardiology |
| Complications | Myocardial infarction, unstable angina |
Angina, also known as angina pectoris, is chest pain or pressure, usually caused by insufficient blood flow to the heart muscle (myocardium).[2] It is most commonly a symptom of coronary artery disease.[2]
Angina is typically the result of partial obstruction or spasm of the arteries that supply blood to the heart muscle.[3] The main mechanism of coronary artery obstruction is atherosclerosis as part of coronary artery disease. Other causes of angina include abnormal heart rhythms, heart failure and, less commonly, anemia.[4] The term derives from Latin angere 'to strangle' and pectus 'chest', and can therefore be translated as "a strangling feeling in the chest".
There is a relationship between severity of angina and degree of oxygen deprivation in the heart muscle. However, the severity of angina does not always match the degree of oxygen deprivation to the heart or the risk of a heart attack (myocardial infarction). Some people may experience severe pain even though there is little risk of a heart attack whilst others may have a heart attack and experience little or no pain.[5][6] In some cases, angina can be quite severe. Worsening angina attacks, sudden-onset angina at rest, and angina lasting more than 15 minutes are symptoms of unstable angina (usually grouped with similar conditions as the acute coronary syndrome). As these may precede a heart attack, they require urgent medical attention and are, in general, treated similarly to heart attacks.[7]
In the early 20th century, severe angina was seen as a sign of impending death.[8] However, modern medical therapies have improved the outlook substantially. Middle-age patients who experience moderate to severe angina (grading by classes II, III, and IV) have a five-year survival rate of approximately 92%.[9]
Classification
Stable angina
Also known as 'effort angina', this refers to the classic type of angina related to myocardial ischemia. A typical presentation of stable angina is that of chest discomfort and associated symptoms precipitated by some activity (running, walking, etc.) with minimal or non-existent symptoms at rest or after administration of sublingual nitroglycerin.[10] Symptoms typically diminish several minutes after activity and recur when activity resumes. In this way, stable angina may be thought of as being similar to intermittent claudication symptoms. Other recognized precipitants of stable angina include cold weather, heavy meals, and emotional stress.
Unstable angina
Unstable angina (UA) (also "crescendo angina"; this is a form of acute coronary syndrome) is defined as angina pectoris that changes or worsens.[11]
It has at least one of these three features:[12]
- it occurs at rest (or with minimal exertion), usually lasting more than 10 minutes
- it is severe and of new-onset (i.e., within the prior 4–6 weeks)
- it occurs with a crescendo pattern (i.e., distinctly more severe, prolonged, or frequent than before).
UA may occur often unpredictably and even at rest, which may be a serious indicator of an impending heart attack. The primary factor differentiating unstable angina from stable angina (other than symptoms) is the underlying pathophysiology of the atherosclerosis. The pathophysiology of unstable angina is the reduction of coronary blood flow due to transient platelet aggregation on apparently normal endothelium, coronary artery spasms, or coronary thrombosis.[13][14]
The process starts with atherosclerosis, progresses through inflammation to yield an active unstable plaque, which undergoes thrombosis and results in acute myocardial ischemia, which, if not reversed, results in cell necrosis (infarction).[14] Studies show that 64% of all unstable anginas occur between 22:00 and 08:00 when patients are at rest.[14][15]
In stable angina, the developing atheroma (a fatty plaque) is protected with a fibrous cap. This cap may rupture in unstable angina, allowing blood clots to precipitate and further decrease the area of the coronary vessel's lumen or the interior open space within an artery. This explains why, in many cases, unstable angina develops independently of activity.[14]
Microvascular angina
Microvascular angina, also known as cardiac syndrome X, is characterized by angina-like chest pain, in the context of normal epicardial coronary arteries (the largest vessels on the surface of the heart, prior to significant branching) on angiography. The original definition of cardiac syndrome X also mandated that ischemic changes on exercise (despite normal coronary arteries) were displayed, as shown on cardiac stress tests.[16] The primary cause of microvascular angina is unknown, but factors apparently involved are endothelial dysfunction and reduced flow (perhaps due to spasm) in the tiny "resistance" blood vessels of the heart.[17] Since microvascular angina is not characterized by major arterial blockages, it is harder to recognize and diagnose.[18][19][20]
Microvascular angina was previously considered a rather benign condition, but more recent data has changed this attitude. Studies, including the Women's Ischemia Syndrome Evaluation (WISE), suggest that microvascular angina is part of the pathophysiology of ischemic heart disease, perhaps explaining the higher rates of angina in females than in males, as well as their predilection towards ischemia and acute coronary syndromes in the absence of obstructive coronary artery disease.[21]
Signs and symptoms

Angina pectoris can be quite painful, but many patients with angina complain of chest discomfort rather than actual pain: the discomfort is usually described as a pressure, heaviness, tightness, squeezing, burning, or choking sensation. Apart from chest discomfort, anginal pains may also be experienced in the epigastrium (upper central abdomen), back, neck area, jaw, or shoulders. This is explained by the concept of referred pain and is because the spinal level that receives visceral sensation from the heart simultaneously receives cutaneous sensation from parts of the skin specified by that spinal nerve's dermatome, without an ability to discriminate the two. Typical locations for referred pain are arms (often inner left arm), shoulders, and neck into the jaw. Angina is typically precipitated by exertion or emotional stress. It is exacerbated by having a full stomach and by cold temperatures. Pain may be accompanied by breathlessness, sweating, and nausea in some cases. In this case, the pulse rate and the blood pressure increases. Chest pain lasting only a few seconds is normally not angina (such as precordial catch syndrome).
Myocardial ischemia comes about when the myocardium (the heart muscle) receives insufficient blood and oxygen to function normally either because of increased oxygen demand by the myocardium or because of decreased supply to the myocardium. This inadequate perfusion of blood and the resulting reduced delivery of oxygen and nutrients are directly correlated to blocked or narrowed blood vessels.
Some experience "autonomic symptoms" (related to increased activity of the autonomic nervous system) such as nausea, vomiting, and pallor.
Major risk factors for angina include cigarette smoking, diabetes, high cholesterol, high blood pressure, sedentary lifestyle, and family history of premature heart disease.
A variant form of angina—Prinzmetal's angina—occurs in patients with normal coronary arteries or insignificant atherosclerosis. It is believed caused by spasms of the artery. It occurs more in younger women.[22]
Coital angina, also known as angina d'amour, is angina subsequent to sexual intercourse.[23] It is generally rare, except in patients with severe coronary artery disease.[23]
Cause
Major risk factors
- Age (≥ 45 years for men, ≥ 55 for women)
- Smoking
- Diabetes mellitus
- Dyslipidemia
- Family history of premature cardiovascular disease (males <55 years, females <65 years old)
- Hypertension
- Kidney disease (microalbuminuria or GFR<60 mL/min)
- Obesity (BMI ≥ 30 kg/m2)
- Physical inactivity
- Prolonged psychosocial stress[24]
Routine counseling of adults by physicians to advise them to improve their diet and increase their physical activity has, in general, been found to induce only small changes in actual behavior. Therefore, as of 2012, The U.S. Preventive Services Task Force does not recommend routine lifestyle counseling of all patients without known cardiovascular disease, hypertension, hyperlipidemia, or diabetes, and instead recommends selectively counseling only those patients who seem most ready to make lifestyle changes and using available time with other patients to explore other types of intervention that would be more likely to have a preventative impact.[25]
- Conditions that exacerbate or provoke angina[26]
- Medications
- Vasodilators
- Excessive thyroid hormone replacement
- Vasoconstrictors
- Polycythemia, which thickens the blood, slowing its flow through the heart muscle
- Hypothermia
- Hypervolemia
- Hypovolemia
One study found that smokers with coronary artery disease had a significantly increased level of sympathetic nerve activity when compared to those without. This is in addition to increases in blood pressure, heart rate, and peripheral vascular resistance associated with nicotine, which may lead to recurrent angina attacks. In addition, the Centers for Disease Control and Prevention (CDC) reports that the risk of CHD (Coronary heart disease), stroke, and PVD (Peripheral vascular disease) is reduced within 1–2 years of smoking cessation. In another study, it was found that, after one year, the prevalence of angina in smokingmales under 60 after an initial attack was 40% less in those having quit smoking compared to those that continued. Studies have found that there are short-term and long-term benefits to smoking cessation.[27][28][29][30]
Other medical problems
- Esophageal disorders
- Gastroesophageal reflux disease (GERD)
- Hyperthyroidism
- Hypoxemia
- Profound anemia
- Uncontrolled hypertension
Other cardiac problems
Myocardial ischemia can result from:
- a reduction of blood flow to the heart that can be caused by stenosis, spasm, or acute occlusion (by an embolus) of the heart's arteries.
- resistance of the blood vessels. This can be caused by narrowing of the blood vessels; a decrease in radius.[33] Blood flow is proportional to the radius of the artery to the fourth power.[34]
- reduced oxygen-carrying capacity of the blood, due to several factors such as a decrease in oxygen tension and hemoglobin concentration.[35] This decreases the ability of hemoglobin to carry oxygen to myocardial tissue.[36]
Atherosclerosis is the most common cause of stenosis (narrowing of the blood vessels) of the heart's arteries and, hence, angina pectoris. Some people with chest pain have normal or minimal narrowing of heart arteries; in these patients, vasospasm is a more likely cause for the pain, sometimes in the context of Prinzmetal's angina and syndrome X.
Myocardial ischemia also can be the result of factors affecting blood composition, such as the reduced oxygen-carrying capacity of blood, as seen with severe anemia (low number of red blood cells), or long-term smoking.
Pathophysiology
Angina results when there is an imbalance between the heart's oxygen demand and supply. This imbalance can result from an increase in demand (e.g., during exercise) without a proportional increase in supply (e.g., due to obstruction or atherosclerosis of the coronary arteries).
However, the pathophysiology of angina in females varies significantly as compared to males.[37] Non-obstructive coronary disease is more common in females.[38][39]
Diagnosis
Angina should be suspected in people presenting tight, dull, or heavy chest discomfort that is:[40]
- Retrosternal or left-sided, radiating to the left arm, neck, jaw, or back.
- Associated with exertion or emotional stress and relieved within several minutes by rest.
- Precipitated by cold weather or a meal.
Some people present with atypical symptoms, including breathlessness, nausea, or epigastric discomfort, or burning. These atypical symptoms are particularly likely in older people, women, and those with diabetes.[40]
Anginal pain is not usually sharp or stabbing or influenced by respiration. Antacids and simple analgesics do not usually relieve the pain. If chest discomfort (of whatever site) is precipitated by exertion, relieved by rest, and relieved by glyceryl trinitrate, the likelihood of angina is increased.[40]
In angina patients momentarily not feeling any chest pain, an electrocardiogram (ECG) is typically normal unless there have been other cardiac problems in the past. During periods of pain, depression, or elevation of the ST segment may be observed. To elicit these changes, an exercise ECG test ("treadmill test") may be performed, during which the patient exercises to his/her maximum ability before fatigue, breathlessness, or pain intervenes; if characteristic ECG changes are documented (typically more than 1 mm of flat or downsloping ST depression), the test is considered diagnostic for angina. Even constant monitoring of the blood pressure and the pulse rate can lead to some conclusions regarding angina. The exercise test is also useful in looking for other markers of myocardial ischemia: blood pressure response (or lack thereof, in particular, a drop in systolic blood pressure), dysrhythmia, and chronotropic response. Other alternatives to a standard exercise test include a thallium scintigram or sestamibi scintigram (in patients unable to exercise enough for the treadmill tests, e.g., due to asthma or arthritis or in whom the ECG is too abnormal at rest) or stress echocardiography.
In patients in whom such noninvasive testing is diagnostic, a coronary angiogram is typically performed to identify the nature of the coronary lesion, and whether this would be a candidate for angioplasty, coronary artery bypass graft (CABG), treatment only with medication, or other treatments. In hospitalized patients with unstable angina (or the newer term of "high-risk acute coronary syndromes"), those with resting ischaemic ECG changes or those with raised cardiac enzymes such as troponin may undergo coronary angiography directly.
Treatment
Angina pectoris occurs as a result of coronary blood flow insufficiency in the face of increased oxygen demand. The principal goal in the prevention and relief of angina is to limit the oxygen requirement of the heart so it can meet the inadequate oxygen supply derived through the blood supplied from the stenosed or constricted arteries. The main goals of treatment in angina pectoris are relief of symptoms, slowing progression of the disease, and reduction of future events, especially heart attacks and death. Beta blockers (e.g., carvedilol, metoprolol, propranolol) have a large body of evidence in morbidity and mortality benefits (fewer symptoms, less disability, and longer life) and short-acting nitroglycerin medications have been used since 1879 for symptomatic relief of angina.[41] There are differing course of treatments for the patient depending on the type of angina the patient has. However, this second can provide a brief overview of the types of medications provided for angina and the purpose by which they are prescribed.
Beta blockers, specifically B1 adrenergic blockers without intrinsic sympathomimetic activity, are preferred for angina treatment, out of B1 selective and non-selective as well as B1 ISA agents. B1 blockers are cardioselective blocking agents (such as nevibolol, atenolol, metoprolol, bisoprolol, etc.) which result in blocking cAMP in the heart muscle cells. cAMP, which plays a vital role in phosphorylating the ryanodine receptor and LTCC, will usually increase Ca+2 levels in the heart muscle cells, blocking contraction. Therefore, B1 blockade decreases the HR and contraction of the heart muscle, making it demand less oxygen. An important thing to note is that the B1 cardioselective blockers are cardioselective and not cardio-specific. This means that if the beta-adrenergic antagonist is prescribed in higher doses, it can lose the selectivity aspect and begin causing hypertension from B2 adrenergic stimulation of smooth muscle cells. This is why in therapy for patients with angina, the vasodilatory organonitrates complement the use of B-blockers when prescribed the use of angina. The preference for Beta-1 cardioselective blockers is for B1 cardioselective blockers without instrinsic sympathetic activity. Beta blockers with intrinsic sympathetic activity will still do the beta blockade of the heart muscle cells and have a decreased ionotrophic and chronotropic effect, but this effect will be to a lesser extent than if the beta blocker did not have the instrinsic sympathetic activity. A common beta-blocker with ISA prescribed for the treatment of angina is Acebutolol.
Non-selective beta-adrenergic antagonists will yield the same action on B1 receptors, however will also act on B2 receptors. These medications, such as Propranolol and Nadolol, act on B1 receptors on smooth muscle cells as well. B1 blockade occurs in the smooth muscle cells. Specifically cAMP is responsible for inhibiting Myosin Light Kinase, the enzyme responsible for acting on Actin-Myosin. The inhibition of B1 will result in decreased levels of cAMP which will lead to increased levels of Myosin Light Chain Kinase in the smooth muscle cells, the enzyme responsible for acting on Actin-Myosin and leading to contraction of the smooth muscle cell. This increased contraction of the smooth muscle cell from B1 blockade is not desirable since it explains the hypertension that may arise with patients taking that medication.
Calcium channel blockers act to decrease the heart's workload, and thus its requirement for oxygen by blocking the calcium channels of the heart muscle cell. With decreased intracellular calcium, the calcium-troponin complex does not form in the heart muscle cell and it does not contract, therefore reducing the need for oxygen.
The other class of medication that can be used to treat angina are the organic nitrates. Organic nitrates are used extensively to treat angina. They improve coronary blood flow of the coronary arteries (arteries which supply blood to the heart muscle) by reversing and preventing vasospasm, which increases the blood flow to the heart, improving perfusion and oxygen delivery to the heart associated with the pain of angina. These drugs also reduce systemic vascular resistance, of both veins and arteries but the veins to a greater extent. The decrease in the resistance of the arteries and veins decreases the myocardial oxygen demand, which also reduces myocardial oxygen demand. Nitroglycerin is a potent vasodilator that decreases myocardial oxygen demand by decreasing the heart's workload. Nitroglycerin should not be given if certain inhibitors such as sildenafil, tadalafil, or vardenafil have been taken within the previous 12 hours as the combination of the two could cause a serious drop in blood pressure.
Treatments for angina are balloon angioplasty, in which the balloon is inserted at the end of a catheter and inflated to widen the arterial lumen. Stents to maintain the arterial widening are often used at the same time. Coronary bypass surgery involves bypassing constricted arteries with venous grafts. This is much more invasive than angioplasty.
Calcium channel blockers (such as nifedipine (Adalat) and amlodipine), isosorbide mononitrate and nicorandil are vasodilators commonly used in chronic stable angina.[citation needed] A new therapeutic class, called If inhibitor, has recently been made available: Ivabradine provides heart rate reduction without affecting contractility[42] leading to major anti-ischemic and antianginal efficacy. ACE inhibitors are also vasodilators with both symptomatic and prognostic benefit. Statins are the most frequently used lipid/cholesterol modifiers, which probably also stabilize existing atheromatous plaque.[43] Low-dose aspirin decreases the risk of heart attack in patients with chronic stable angina, and was part of standard treatment. However, in patients without established cardiovascular disease, the increase in hemorrhagic stroke and gastrointestinal bleeding offsets any benefits and it is no longer advised unless the risk of myocardial infarction is very high.[44]
Exercise is also a very good long-term treatment for the angina (but only particular regimens – gentle and sustained exercise rather than intense short bursts),[45] probably working by complex mechanisms such as improving blood pressure and promoting coronary artery collateralisation.
Though sometimes used by patients, evidence does not support the use of traditional Chinese herbal products (THCP) for angina.[46]
Identifying and treating risk factors for further coronary heart disease is a priority in patients with angina. This means testing for elevated cholesterol and other fats in the blood, diabetes and hypertension (high blood pressure), and encouraging smoking cessation and weight optimization.
The calcium channel blocker nifedipine prolongs cardiovascular event- and procedure-free survival in patients with coronary artery disease. New overt heart failures were reduced by 29% compared to placebo; however, the mortality rate difference between the two groups was statistically insignificant.[47]
Microvascular angina in women
Women with myocardial ischemia often have either no or atypical symptoms, such as palpitations, anxiety, weakness, and fatigue. Additionally, many females with angina are found to have cardiac ischemia, yet no evidence of obstructive coronary artery disease on cardiac catheterization. Evidence is accumulating that nearly half of females with myocardial ischemia have coronary microvascular disease, a condition often called microvascular angina (MVA). Small intramyocardial arterioles constrict in MVA causing ischemic pain that is less predictable than with typical epicardial coronary artery disease (CAD).
The pathophysiology is complex and still being elucidated, but there is strong evidence that endothelial dysfunction, decreased endogenous vasodilators, inflammation, changes in adipokines, and platelet activation are contributing factors. The diagnosis of MVA may require catheterization during which there is an assessment of the microcirculatory response to adenosine or acetylcholine and measurement of coronary and fractional flow reserve. New techniques include positron emission tomography (PET) scanning, cardiac magnetic resonance imaging (MRI), and transthoracic Doppler echocardiography.
Managing MVA can be challenging, for example, females with this condition have less coronary microvascular dilation in response to nitrates than do those without MVA. Females with MVA often have traditional risk factors for CAD such as obesity, dyslipidemia, diabetes, and hypertension. Aggressive interventions to reduce modifiable risk factors are an important component of management, especially smoking cessation, exercise, and diabetes management. The combination of non-nitrate vasodilators, such as calcium channel blockers and angiotensin-converting enzyme (ACE) inhibitors along with HMG-CoA reductase inhibitors (statins), also is effective in many women, and new drugs, such as Ranolazine and Ivabradine, have shown promise in the treatment of MVA. Other approaches include spinal cord stimulators, adenosine receptor blockade, and psychiatric intervention.[48][49][50][51][52][53]
Suspected angina
Hospital admission for people with the following symptoms is recommended, as they may have unstable angina: pain at rest (which may occur at night), pain on minimal exertion, angina that seems to progress rapidly despite increasing medical treatment. All people with suspected angina should be urgently referred to a chest pain evaluation service, for confirmation of the diagnosis and assessment of the severity of coronary heart disease.[54]
Epidemiology
As of 2010, angina due to ischemic heart disease affects approximately 112 million people (1.6% of the global population) being slightly more common in males than females (1.7% to 1.5%).[55]
In the United States, 10.2 million are estimated to experience angina with approximately 500,000 new cases occurring each year.[10][56] Angina is more often the presenting symptom of coronary artery disease in females than in men. The prevalence of angina rises with increasing age, with a mean age of onset of 62.3 years.[57] After five years post-onset, 4.8% of individuals with angina subsequently died from coronary heart disease. Males with angina were found to have an increased risk of subsequent acute myocardial infarction and coronary heart disease related death than women. Similar figures apply in the remainder of the Western world. All forms of coronary heart disease are much less-common in the Third World, as its risk factors are much more common in Western and Westernized countries; it could, therefore, be termed a disease of affluence.
History
The condition was named "hritshoola" in ancient India and was described by Sushruta (6th century BC).[58]
The first clinical description of angina pectoris was by a British physician Dr. William Heberden in 1768.[59]
References
- ^ "The definition of angina".
- ^ a b "Coronary Heart Disease, Myocardial Infarction, and Stroke — A Public Health Issue | CDC". www.cdc.gov. 31 July 2019. Retrieved 16 January 2022.
- ^ Dorland's Illustrated Medical Dictionary. Philadelphia, PA: Saunders. 2003. p. 82. ISBN 0-7216-0146-4. Retrieved 24 August 2022.
- ^ Perera, Chanaka Aravinda, Biggers, Richard Peters, Robertson, Alan (1 August 2019). "Deceitful red-flag: angina secondary to iron deficiency anaemia as a presenting complaint for underlying malignancy". BMJ Case Reports. 12 (7): e229942. doi:10.1136/bcr-2019-229942. PMC 6677945. PMID 31371333.
- ^ Björck, Lena, Nielsen, Susanne, Jernberg, Tomas, Zverkova-Sandström, Tatiana, Giang, Kok Wai, Rosengren, Annika (26 November 2018). "Absence of chest pain and long-term mortality in patients with acute myocardial infarction". Open Heart. 5 (2): e000909. doi:10.1136/openhrt-2018-000909. PMC 6269644. PMID 30564376. Retrieved 27 August 2022.
- ^ Canto, John G., Goldberg, Robert J., Hand, Mary M. (10 December 2007). "Symptom Presentation of Women With Acute Coronary Syndromes: Myth vs Reality". Archives of Internal Medicine. 167 (22): 2405–2413. doi:10.1001/archinte.167.22.2405. PMID 18071161. Archived from the original on 2022-08-27. Retrieved 27 August 2022.
- ^ American Heart Association (8 November 2021). "Angina (Chest Pain)". American Heart Association. Archived from the original on 27 August 2022. Retrieved 27 August 2022.
- ^ White PD (1931). Heart Disease (1st ed.). Macmillan.
- ^ Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. (April 2007). "Optimal medical therapy with or without PCI for stable coronary disease". The New England Journal of Medicine. 356 (15): 1503–16. doi:10.1056/NEJMoa070829. PMID 17387127.
- ^ a b Tobin KJ (July 2010). "Stable angina pectoris: what does the current clinical evidence tell us?". The Journal of the American Osteopathic Association. 110 (7): 364–70. PMID 20693568. Archived from the original on 2020-03-11. Retrieved 2013-02-07.
- ^ "MerckMedicus: Dorland's Medical Dictionary". Retrieved 2009-01-09.
- ^ "Unstable Angina". www.heart.org. Retrieved 2023-10-23.
- ^ Hombach V, Höher M, Kochs M, Eggeling T, Schmidt A, Höpp HW, et al. (December 1988). "Pathophysiology of unstable angina pectoris--correlations with coronary angioscopic imaging". European Heart Journal. 9 Suppl N: 40–5. doi:10.1093/eurheartj/9.suppl_N.40. PMID 3246255.
- ^ a b c d Simons M (March 8, 2000). "Pathophysiology of unstable angina". Archived from the original on March 30, 2010. Retrieved April 28, 2010.
- ^ "What Is Angina?". National Heart Lung and Blood Institute. Retrieved April 28, 2010.
- ^ Kaski JC, ed. (1999). Chest pain with normal coronary angiograms: pathogenesis, diagnosis and management. Boston: Kluwer. pp. 5–6. ISBN 978-0-7923-8421-2.
- ^ Guyton, Arthur. "Textbook of Medical Physiology" 11th edition. Philadelphia; Elsevier, 2006.[page needed]
- ^ "Cardiac Syndrome X". HeartHealthyWomen.org. 14 August 2022.[unreliable medical source?]
- ^ "Heart Attack and Angina Statistics". Archived from the original on 2010-04-13. Retrieved 2010-04-13. [failed verification].
- ^ "Angina". Texas Heart Institute. October 2012. Archived from the original on 2014-08-17. Retrieved 2010-05-04.
- ^ Gulati M, Shaw LJ, Bairey Merz CN (March 2012). "Myocardial ischemia in women: lessons from the NHLBI WISE study". Clinical Cardiology. 35 (3): 141–8. doi:10.1002/clc.21966. PMC 3297966. PMID 22389117.
- ^ Sun H, Mohri M, Shimokawa H, Usui M, Urakami L, Takeshita A (March 2002). "Coronary microvascular spasm causes myocardial ischemia in patients with vasospastic angina". Journal of the American College of Cardiology. 39 (5): 847–51. doi:10.1016/S0735-1097(02)01690-X. PMID 11869851.
- ^ a b Levine GN, Steinke EE, Bakaeen FG, Bozkurt B, Cheitlin MD, Conti JB, et al. (February 2012). "Sexual activity and cardiovascular disease: a scientific statement from the American Heart Association". Circulation. 125 (8): 1058–72. doi:10.1161/CIR.0b013e3182447787. PMID 22267844.
- ^ Linden W, Stossel C, Maurice J (April 1996). "Psychosocial interventions for patients with coronary artery disease: a meta-analysis". Archives of Internal Medicine. 156 (7): 745–52. doi:10.1001/archinte.1996.00440070065008. PMID 8615707.
- ^ Moyer VA (September 2012). "Behavioral counseling interventions to promote a healthful diet and physical activity for cardiovascular disease prevention in adults: U.S. Preventive Services Task Force recommendation statement". Annals of Internal Medicine. 157 (5): 367–71. doi:10.7326/0003-4819-157-5-201209040-00486. PMID 22733153.
- ^ Wells B, DiPiro J, Schwinghammer T, DiPiro C (2008). Pharmacotherapy Handbook (7th ed.). New York: McGraw-Hill. p. 140. ISBN 978-0-07-148501-2.
- ^ "Health Benefits of Cessation". U.S. Centers for Disease Control and Prevention. January 3, 2013.
- ^ Daly LE, Graham IM, Hickey N, Mulcahy R (October 1985). "Does stopping smoking delay onset of angina after infarction?". British Medical Journal. 291 (6500): 935–7. doi:10.1136/bmj.291.6500.935. PMC 1417185. PMID 3929970.
- ^ Daly LE, Mulcahy R, Graham IM, Hickey N (July 1983). "Long term effect on mortality of stopping smoking after unstable angina and myocardial infarction". British Medical Journal. 287 (6388): 324–6. doi:10.1136/bmj.287.6388.324. PMC 1548591. PMID 6409291.
- ^ Shinozaki N, Yuasa T, Takata S (May 2008). "Cigarette smoking augments sympathetic nerve activity in patients with coronary heart disease". International Heart Journal. 49 (3): 261–72. doi:10.1536/ihj.49.261. PMID 18612184.
- ^ Gibbons RJ, Abrams J, Chatterjee K, Daley J, Deedwania PC, Douglas JS, et al. (January 2003). "ACC/AHA 2002 guideline update for the management of patients with chronic stable angina--summary article: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on the Management of Patients With Chronic Stable Angina)". Journal of the American College of Cardiology. 41 (1): 159–68. doi:10.1016/S0735-1097(02)02848-6. PMID 12570960.
- ^ Fraker TD, Fihn SD, Gibbons RJ, Abrams J, Chatterjee K, Daley J, et al. (December 2007). "2007 chronic angina focused update of the ACC/AHA 2002 guidelines for the management of patients with chronic stable angina: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Writing Group to develop the focused update of the 2002 guidelines for the management of patients with chronic stable angina". Journal of the American College of Cardiology. 50 (23): 2264–74. doi:10.1016/j.jacc.2007.08.002. PMID 18061078.
- ^ Kusumoto FM (2009-10-20). "Chapter 10: Cardiovascular Disorders: Heart Disease". In McPhee SJ, Hammer GD (eds.). Pathophysiology of Disease: An Introduction to Clinical Medicine (6th ed.). McGraw-Hill Education. p. 276. ISBN 978-0-07-162167-0. Archived from the original on 2011-07-27. Retrieved 2010-04-28.
- ^ Michel T (2005-09-13). "Treatment of Myocardial Ischemia". In Brunton LL, Lazo JS, Parker KL (eds.). Goodman & Gilman's The Pharmacological Basis of Therapeutic (11th ed.). McGraw-Hill Companies,Incorporated. p. 823. ISBN 978-0-07-142280-2.
- ^ Podrid PJ (November 28, 2012). "Pathophysiology and clinical presentation of ischemic chest pain". UpToDate. Wolters Kluwer.(registration required)
- ^ Traverso M (8 August 2004). "The Crucial Role of Iron in the Body". Washington University in St Louis. Archived from the original on 7 June 2010.
- ^ Vaccarino V (March 2010). "Ischemic heart disease in : many questions, few facts". Circulation: Cardiovascular Quality and Outcomes. 3 (2): 111–5. doi:10.1161/CIRCOUTCOMES.109.925313. PMC 3012351. PMID 20160161.
- ^ Shaw LJ, Merz CN, Pepine CJ, Reis SE, Bittner V, Kip KE, et al. (August 2006). "The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health--National Heart, Lung, and Blood Institute--sponsored Women's Ischemia Syndrome Evaluation". Circulation. 114 (9). Women's Ischemia Syndrome Evaluation (WISE), Investigators: 894–904. doi:10.1161/CIRCULATIONAHA.105.609990. PMID 16923752.
- ^ Banks K, Lo M, Khera A (February 2010). "Angina in Women without Obstructive Coronary Artery Disease". Current Cardiology Reviews. 6 (1): 71–81. doi:10.2174/157340310790231608. PMC 2845797. PMID 21286281.
- ^ a b c NHS Clinical Knowledge Summaries (2009) Angina - stable. "Clinical topic - Angina". Archived from the original on 2010-03-10. Retrieved 2010-01-04. Date site accessed: 04/01/2009
- ^ Sneader W (2005). Drug discovery: a history. Wiley. ISBN 978-0-471-89980-8.[page needed]
- ^ Sulfi S, Timmis AD (February 2006). "Ivabradine -- the first selective sinus node I(f) channel inhibitor in the treatment of stable angina". International Journal of Clinical Practice. 60 (2): 222–8. doi:10.1111/j.1742-1241.2006.00817.x. PMC 1448693. PMID 16451297.
- ^ Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al. (April 2006). "Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial". JAMA. 295 (13): 1556–65. doi:10.1001/jama.295.13.jpc60002. PMID 16533939.
- ^ Barnett H, Burrill P, Iheanacho I (April 2010). "Don't use aspirin for primary prevention of cardiovascular disease". BMJ. 340: c1805. doi:10.1136/bmj.c1805. PMID 20410163. S2CID 3137720.
- ^ Ades PA, Waldmann ML, Poehlman ET, Gray P, Horton ED, Horton ES, et al. (August 1993). "Exercise conditioning in older coronary patients. Submaximal lactate response and endurance capacity". Circulation. 88 (2): 572–7. doi:10.1161/01.CIR.88.2.572. PMID 8339420.
- ^ Zhuo Q, Yuan Z, Chen H, Wu T (May 2010). "Traditional Chinese herbal products for stable angina". The Cochrane Database of Systematic Reviews. 2010 (5): CD004468. doi:10.1002/14651858.cd004468.pub2. PMC 6718232. PMID 20464731.
- ^ Poole-Wilson PA, Lubsen J, Kirwan BA, van Dalen FJ, Wagener G, Danchin N, et al. (Coronary disease Trial Investigating Outcome with Nifedipine gastrointestinal therapeutic system investigators) (2004). "Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with stable angina requiring treatment (ACTION trial): randomised controlled trial". Lancet. 364 (9437): 849–57. doi:10.1016/S0140-6736(04)16980-8. PMID 15351192. S2CID 12795811.
- ^ Celik T, Ozturk C, Balta S, Demirkol S, Iyisoy A (September 2016). "Coronary microvascular dysfunction in patients with cardiac syndrome X: Ongoing debate". International Journal of Cardiology. 218: 233–234. doi:10.1016/j.ijcard.2016.05.050. PMID 27236120.
- ^ Cattaneo M, Porretta AP, Gallino A (February 2015). "Ranolazine: Drug overview and possible role in primary microvascular angina management". International Journal of Cardiology. 181: 376–81. doi:10.1016/j.ijcard.2014.12.055. PMID 25555283.
- ^ Lanza GA, Careri G, Stazi A, Villano A, De Vita A, Aurigemma C, et al. (June 2016). "Clinical Spectrum and Outcome of Patients With Non-ST-Segment Elevation Acute Coronary Syndrome and No Obstructive Coronary Atherosclerosis". Circulation Journal. 80 (7): 1600–6. doi:10.1253/circj.CJ-16-0145. PMID 27245239.
- ^ Marinescu MA, Löffler AI, Ouellette M, Smith L, Kramer CM, Bourque JM (February 2015). "Coronary microvascular dysfunction, microvascular angina, and treatment strategies". JACC. Cardiovascular Imaging. 8 (2): 210–20. doi:10.1016/j.jcmg.2014.12.008. PMC 4384521. PMID 25677893.
- ^ Selthofer-Relatić K, Bošnjak I, Kibel A (2016). "Obesity Related Coronary Microvascular Dysfunction: From Basic to Clinical Practice". Cardiology Research and Practice. 2016: 8173816. doi:10.1155/2016/8173816. PMC 4820617. PMID 27092288.
- ^ Titterington JS, Hung OY, Wenger NK (March 2015). "Microvascular angina: an update on diagnosis and treatment". Future Cardiology. 11 (2): 229–42. doi:10.2217/fca.14.79. PMID 25760881.
- ^ "Suspected angina". NHS Clinical Knowledge Summaries. U.K. National Institute for Health and Clinical Excellence. 2009. Archived from the original on December 14, 2010.
- ^ Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2163–96. doi:10.1016/S0140-6736(12)61729-2. PMC 6350784. PMID 23245607.
- ^ Rosamond W, Flegal K, Furie K, Go A, Greenlund K, Haase N, et al. (January 2008). "Heart disease and stroke statistics--2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee". Circulation. 117 (4): e25-146. doi:10.1161/CIRCULATIONAHA.107.187998. PMID 18086926.
- ^ Buckley BS, Simpson CR, McLernon DJ, Murphy AW, Hannaford PC (August 2009). "Five year prognosis in patients with angina identified in primary care: incident cohort study". BMJ. 339: b3058. doi:10.1136/bmj.b3058. PMC 2722695. PMID 19661139.
- ^ Dwivedi G, Dwivedi S (2007). "Sushruta – the Clinician – Teacher par Excellence" (PDF). The Indian Journal of Chest Diseases and Allied Sciences. 49: 243–4. Archived from the original (PDF) on 2008-10-10.
- ^ "Angina Pectoris: The Eighteenth-Century Origins of Angina Pectoris: Predisposing Causes, Recognition, and Aftermath". JAMA. 288 (15): 1917–1918. 2002-10-16. doi:10.1001/jama.288.15.1917-JBK1016-3-1. ISSN 0098-7484.
External links
- Treatment of stable angina recommendations for patients in layman's terms
- British Heart Foundation - Angina Archived 2017-12-22 at the Wayback Machine
- Angina Pectoris Animation Video 3D Archived 2011-02-21 at the Wayback Machine
- Guidelines on the management of stable angina pectoris - European Society of Cardiology
- Heart Attack and Angina Statistics by American Heart Association: Final 2006 statistics for the United States
- . Encyclopædia Britannica. Vol. II (9th ed.). 1878. p. 29.

















