Integrative diagnostics: The time is now—a report from the International Society for Strategic Studies in Radiology
| Full article title | Integrative diagnostics: The time is now—a report from the International Society for Strategic Studies in Radiology |
|---|---|
| Journal | Insights into Imaging |
| Author(s) | Beauchamp, Norman J.; Bryan R. Nick; Bui, Marilyn M.; Krestin, Gabriel P.; McGinty, Geraldine B.; Meltzer, Carolyn C.; Neumaier, Michael |
| Author affiliation(s) | Michigan State University, University of Pennsylvania, Moffitt Cancer Center and Research Institute, University Medical Center Rotterdam, Weill Cornell Medicine, University of Southern California, University of Heidelberg |
| Primary contact | Email: robert dot bryan at pennmedicine dot upenn dot edu |
| Year published | 2022 |
| Volume and issue | 14 |
| Article # | 54 |
| DOI | 10.1186/s13244-023-01379-9 |
| ISSN | 1869-4101 |
| Distribution license | Creative Commons Attribution 4.0 International |
| Website | https://insightsimaging.springeropen.com/articles/10.1186/s13244-023-01379-9 |
| Download | https://insightsimaging.springeropen.com/counter/pdf/10.1186/s13244-023-01379-9.pdf (PDF) |
Abstract
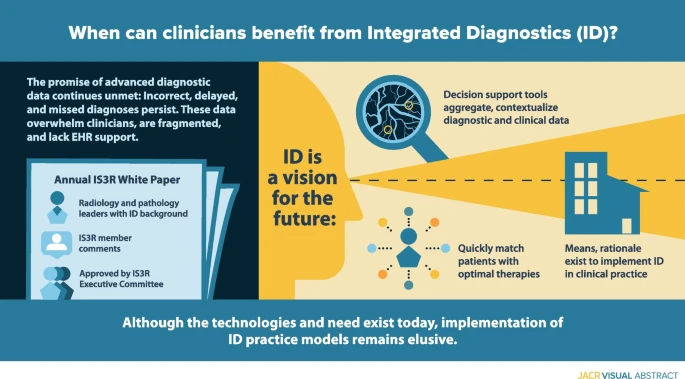
Enormous recent progress in diagnostic testing can enable more accurate diagnosis and improved clinical outcomes. Yet these tests are increasingly challenging and frustrating; the volume and diversity of results may overwhelm the diagnostic acumen of even the most dedicated and experienced clinician. Because they are gathered and processed within the “silo” of each diagnostic discipline, diagnostic data are fragmented, and the electronic health record (EHR) does little to synthesize new and existing data into usable information. Therefore, despite great promise, diagnoses may still be incorrect, delayed, or never made. Integrative diagnostics represents a vision for the future, wherein diagnostic data, together with clinical data from the EHR, are aggregated and contextualized by informatics tools to direct clinical action. Integrative diagnostics has the potential to identify correct therapies more quickly, modify treatment when appropriate, and terminate treatment when not effective, ultimately decreasing morbidity, improving outcomes, and avoiding unnecessary costs. Radiology, laboratory medicine, and pathology already play major roles in medical diagnostics. Our specialties can increase the value of our examinations by taking a holistic approach to their selection, interpretation, and application to the patient’s care pathway. We have the means and rationale to incorporate integrative diagnostics into our specialties and guide its implementation in clinical practice.
The following overall points can be made about this research:
- Despite being an overall boon to clinical diagnosis, increasingly voluminous, diverse, and fragmented diagnostic data can overwhelm physicians and frustrate patients.
- Data are gathered and processed within “silos” of the diagnostic disciplines, including radiology and pathology. The EHR does little to intelligently organize and synthesize these disparate data to facilitate diagnosis.
- Integrative diagnostics envisions a process in which data from the entire arsenal of in vivo and in vitro diagnostics, together with clinical data from the EHR, are aggregated and contextualized to enhance diagnosis and direct clinical action.
Keywords: diagnostics, integrative diagnostics, radiology, pathology, informatics, clinical informatics
Background
Despite digital imaging, widespread adoption of electronic health records (EHRs), and advances in precision medicine tools, diagnosis often remains a fragmented and frustrating process for clinicians and patients. Data are still gathered and presented asynchronously, and EHRs do little to organize and synthesize information. Although team practice, such as tumor boards, is increasing, routine physician interaction is limited by clinical workflow, high volumes, and information technology (IT) boundaries. Despite an abundance of relevant diagnostic data, diagnoses may be incorrect, delayed, or never made. Allegations of diagnostic errors account for 28% of malpractice cases in the United States.[1] Experts estimate a diagnostic error rate of 10% to 15%, with 40,000–80,000 preventable deaths each year.[2][3] As physicians and diagnosticians, it is our responsibility to minimize these errors. Integrative diagnostics (ID) has been proposed as one means to reduce diagnostic errors.
Method
This paper is designed to address ID from the perspectives of radiology and our sister diagnostic specialty, pathology. The paper was developed in response to a request for proposal from the International Society of Strategic Studies in Radiology (IS3R) to its members for an annual white paper to foster its mission “to actively shape the future of medical imaging and image-guided therapies by leveraging the knowledge and influence of world leaders in these disciplines and related industries.” Proposals from self-organized writing groups were reviewed by the IS3R Publications Committee, with the final selection approved for drafting by the IS3R Executive Committee. Our writing group was designed to include departmental and institutional leaders in radiology and pathology who have interest and experience in ID. After preliminary approval by the Publications Committee, the draft paper was posted to the entire IS3R membership for comments, which were incorporated into this final document. This paper was approved for internal dissemination and publication by the IS3R Executive Committee.
What is ID?
More than seven billion diagnostic examinations are performed each year in the United States, influencing 70% of health care decisions.[4] Although diagnostic tests differ in personnel, infrastructure, and technology, they have a shared commonality: providing data for clinical diagnosis.[5] ID has been proposed to better manage, organize, and present diagnostic data and bridge intellectual silos. ID represents a convergence of imaging, pathology, and clinical laboratory medicine, plus advanced levels of IT.[6] In this framework, integrated (versus isolated) practices plus clinical decision support (CDS) tools drive appropriate care. Data from the entire diagnostic arsenal are aggregated to enhance insights, and EHRs present information in a consumable way to facilitate collaborative decision making and accurate clinical diagnosis. ID uses medical informatics (in which data are data, regardless of their nature or source) to organize and analyze vast, disparate diagnostic data sets to achieve timely and accurate diagnosis, precise therapeutics, accurate assessment of prognosis, and maintenance of population health.[7]
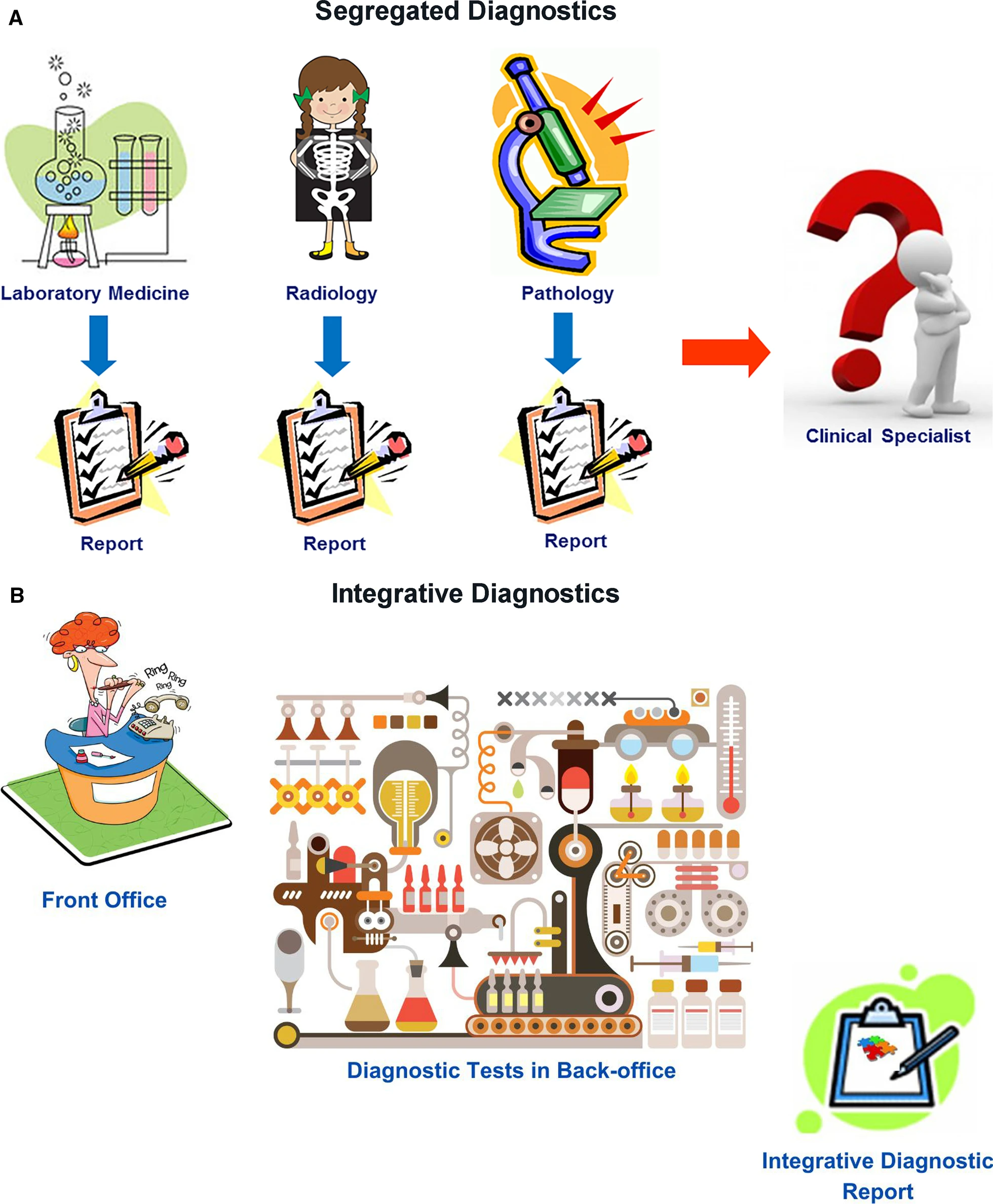
Radiology, clinical laboratories, and pathology departments, which perform the preponderance of diagnostic tests, currently play a central role in medical diagnostics. However, our disciplines have not worked as an integrated unit. Rather, we are islands of vast data and extraordinary intradisciplinary expertise separated from one another and from our clinical colleagues by informatics, physical, and specialty barriers. We have not integrated our data or communicated them in a coordinated fashion to our clinical colleagues, instead expecting clinicians to integrate and interpret these data themselves. Although of immense potential value, our petabytes of data are increasingly overwhelming providers and systems as we “throw our work over the fence” and hope that someone figures out what it all means (Fig. 1A). It is no longer possible for individual health care providers to perform this complex task. ID offers a helping hand.
|
In ID, radiologists, pathologists, and other diagnosticians work as teams with shared access to continuously updated patient data, from which experts and CDS tools extract relevant clinical information and formulate dynamic differential diagnosis and management pathways (Fig. 1B). Given our in-depth knowledge of our test data, understanding of the pathobiochemical and physiological basis of our diagnostic findings, technological skills, and strong informatics resources and expertise, the practices of radiology and pathology should strive for leadership roles in the ID environment.
Predictive analytic tools based on aggregated clinical data can streamline care pathways so that appropriate diagnostic tests (including those performed by radiology, laboratory medicine, and pathology) are expedited on the basis of reason for referral, even in advance of a patient’s visit with a provider. This requires real-time data entry from all sources, continual analytics, and timely interactive communication among laboratories, providers, and patients. Triaging patients in this manner could streamline and more appropriately prioritize health care access. For example, by identifying patients who need to be seen sooner, a decrease in wait times for specialists would provide reassurance to patients earlier in their care journey and prevent them from turning to high-cost settings such as the emergency department for care. ID could direct patients to the correct therapy sooner, modify treatment when appropriate, and terminate it when not effective, ultimately decreasing morbidity, improving outcomes, and avoiding unnecessary cost. Earlier access and more appropriate care are increasingly rewarded in value-based care payment arrangements. Additionally, ID could assess information that affects both individual patient well-being and population health, including identification of emerging infections, antibiotic resistance, exposure to toxic substances, and chemical or biologic threats.
Despite a clear need and sound theoretical reasons for expanding the role of radiologists and pathologists in ID, real-world efforts remain meager. Our purpose is to stimulate more ID activity in our specialties by presenting the rationale for such efforts, highlighting successful ID programs that might be emulated at other sites, and recommending specific endeavors that are feasible now and should be prioritized in our departments and institutions.
The ID process
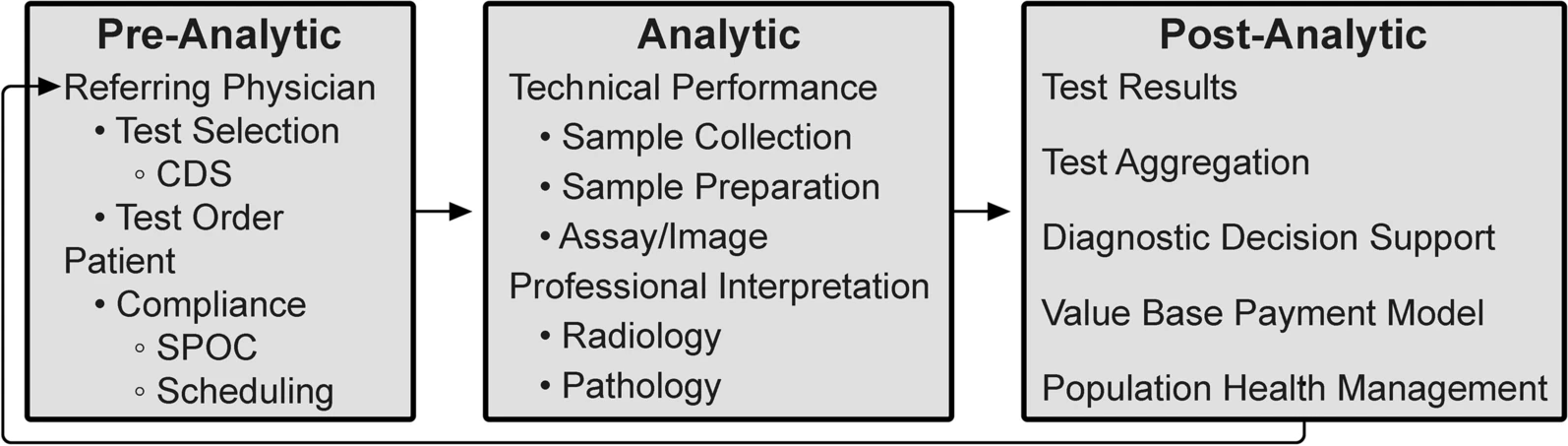
As outlined by the Institute of Medicine Committee on Diagnostic Error in Health Care, the diagnostic examination process is divided into three phases: pre-analytic, analytic, and post-analytic.[7][8] (Fig. 2)
|
The analytic phase is the least susceptible to errors because of attention to technical performance and procedural standards, rigorous internal management and external quality assessment, and precise quantitative measurements. In contrast, our relative inattention to the pre- and post-analytic phases now warrants modification. In laboratory medicine, the analytic phase accounts for approximately 25% of total effort and workflow, the pre-analytic phase for 57%, and the post-analytic phase for 17%.[9] A disease process that requires inputs from multiple diagnostic disciplines is typically interrogated in a stepwise and discontinuous way. Although this is sometimes unavoidable (including subsequent testing whose utility only becomes apparent on the basis of preceding tests), the fragmented, sequential nature of the diagnostic process can cause treatment delays with negative impacts on outcomes.[10] ID can accelerate medical diagnosis, transforming this discontinuous, slow, and fragmented approach into a highly coordinated process with faster information flow through these test phases.
In the pre-examination phase, the referring provider is responsible for performing and/or requesting the most appropriate examinations. In an estimated 10 to 15% of cases, the referring provider needs, and would value, assistance with these decisions. Inappropriate laboratory testing involves both under- and overutilization and occurs in 20 to 30% of cases.[11] Extra support may be needed for primary care providers, who see a wide variety of patients and diseases.[12] Modern health care informatics can help providers request the most appropriate examinations by integrating CDS tools into clinical workflow.[13] For example, use of a real-time radiology appropriateness CDS application decreased inappropriate utilization of brain and spine MRI and sinus CT[14], and computer-generated reminders to clinicians in Kenya improved CD4 laboratory monitoring of patients with HIV infection.[15] CDS tools should be available on platforms that integrate seamlessly into providers’ workflow without adding unnecessary steps, and the appropriate use criteria underpinning these tools must be evidence-based. Feedback to providers must be supportive and advance learning, rather than being punitive. Additionally, CDS systems should be adapted to local circumstances, including local patient demographics and resources (such as the availability of diagnostic test equipment and the competencies of diagnosticians). CDS systems must also be capable of incorporating all relevant patient data. Moreover, CDS should be “integrated,” reflecting not only the appropriateness of a single diagnostic discipline but also the benefit of combinations of tests across disciplines.
Although referring physicians are responsible for maximizing the likelihood that patients will get needed examinations, approximately 20% of requested examinations in the United States are never performed.[16] Well-designed health care systems using contemporary, web-connected logistic support tools can improve this by coordinating examination times across disciplines at sites that match patients’ circumstances and preferences to local health care resources. Point-of-care (POC) testing and service increases patient test completion, satisfaction, and clinical outcomes, although it presents efficiency and quality control (QC) challenges. POC laboratory testing has improved clinical outcomes in influenza and pneumonia, HIV infection, heart attack, and strep throat.[17] In Berlin, the use of mobile stroke units with CT scans and POC laboratory tests resulted in decreased time to treatment and lower global disability at three-month follow-up.[18]
The analytic phase of the diagnostic process centers on the performance of each specific examination, which are currently relatively independent events. Most picture archiving and communication systems (PACS) and radiology information systems (RIS) are separate from laboratory information systems (LIS), resulting in each pathologist and radiologist interpreting their own studies without easy access to the others’ results. Bridging this disconnect should be a radiology and pathology IT priority. Diagnostic accuracy and management recommendations are improved when examinations are tailored and interpreted using knowledge from previous tests. Modern informatics, through optimizing the EHR, should make the complete medical record available to every examiner at the time of an examination, along with appropriate management guidelines. Each study’s unique information should be intelligently and intuitively encapsulated in each sequential result. For example, POC CDS for management of incidental lung nodules improved adherence to nationally recommended guidelines for follow-up.[19]
The post-analytic phase of diagnostics initially focuses on the application of test results to the individual patient’s diagnosis and care plan. The aggregation and diagnostic inferences from all of a patient’s examinations leads to the most accurate and specific diagnosis. Examination results should be promptly and intuitively incorporated into the EHR and made easily available to health care providers and the patient. Until the past decade, these medical data were analyzed by a single or small number of providers, primarily using heuristics. Although an invaluable human thought process, heuristics takes shortcuts in reasoning, may not use all available data, and has well-known sources of error, including cognitive, selective, and availability biases.[20] Furthermore, heuristics suffers reduced accuracy and efficiency with increasing volumes and diversity of data types and greater task complexity.
Deficiencies in current practice and EHRs extend from the most basic error—missing data—to data overload, as with radiopathogenomics. For example, in a Veterans Affairs setting, 30% of providers reported encountering at least one patient with a missed test result over the previous two weeks that caused a delay in diagnosis or treatment.[21] Tumor boards, with their extensive clinical, imaging, laboratory, and anatomic pathology content, may represent the epitome of data overload. No single human can master all the information of even one patient in any reasonable period of time, which was the topic of an RSNA/American Association of Physicists in Medicine symposium on ID in 2019.[22] The current explosion of remote health monitoring tools and diagnostic tests with exponentially larger data units can easily overwhelm a single astute physician. It is estimated that every patient generates 80 MB of data each year, and the volume of health care data is predicted to increase faster than any other business sector.[23][24] ID can bring more human and computational resources to bear on these essentially raw data to yield useful information to diagnose and treat individual patient problems as well as address population disease and health management.[25]
An intelligent informatics infrastructure leveraging all these individual and population data can greatly augment the traditional human analysis. Integrated structured reports with discrete data are critical for data aggregation, which, in conjunction with outcome data, allows the development and optimization of front-end CDS systems. CDS tools, incorporating artificial intelligence (AI) and machine learning (ML) methodology, can provide referring providers with real-time probabilistic differential diagnoses for individual patients and enable the development of management paradigms for specific diseases and large populations.[26] Unfortunately, many CDS systems are monodisciplinary, prematurely obsolete, and incompatible with efficient clinical workflow. Modern health care informatics must develop fully integrated CDS tools that are multidisciplinary, continuously updated, and adapted to the local situation. These new management paradigms can close the loop from the post-analytic back to the pre-analytic phase by suggesting the most appropriate examinations for the referring physician’s next patient with a similar problem set. Furthermore, this information can help health care systems identify their most burdensome and needy patients for proactive health care management.
In the United States, the 21st Century Cures Act emphasizes the patient’s role in the post-analytic phase. The program rule on interoperability, information blocking, and Office of National Health Coordinator (ONHC) health IT certification, which implements this act, requires that health care providers give patients access without charge to all the health information in their EHR “without delay.”[27] This legislative directive, predicated on evidence that optimal diagnosis and treatment are enhanced by the convenient availability of patients’ medical records to their physicians, will further drive the aggregation of medical information, regardless of initial source or current repository. This initiative should better enable all physicians involved in a patient’s care to have immediate access to all of that patient’s health care information. Although providing invaluable information to providers, including radiologists and pathologists, the technical and legal demands of this act on provider practices, health systems, and IT vendors will be significant. The requirement that all components of the EHR be promptly provided to the patient, including all laboratory, anatomic pathology, and radiology reports, presents a communication challenge and an opportunity for ID. We will have to modify our reports for patients’ consumption through health care portals, offering the opportunity to integrate and summarize test results for patients and referring physicians.
ID in tandem with radiology and pathology: “In vivo” meets “In vitro”
In 2020, the European Society of Radiology and the European Federation of Laboratory Medicine signed a memorandum of understanding confirming international support of ID between both disciplines.[28] Underlying this alliance is the favorable complementarity of diagnostic scope and data generated by the two fields. Modern imaging technologies provide high-resolution morphologic information but limited information on tissue metabolism and potential function and no systems information. In contrast, clinical laboratory medicine measures thousands of biochemical and molecular markers with moderate to high tissue specificity in various bodily fluids, but it rarely gives the pinpoint morphologic information that radiology can provide. For example, molecular biomarkers can sensitively indicate the presence of minute brain lesions, but these markers cannot localize a defect within the organ, assess the size of a lesion, or even count the number of lesions, functions that are easily provided by high-resolution in vivo imaging.[29]
Table 1 demonstrates the clinical potential of ID between imaging and laboratory medicine. Each diagnosis or medical condition requires the results of a specific set of clinical, laboratory, radiology, and pathology tests to achieve a precise diagnosis. To make efficient use of our siloed data for ID, we must define interdisciplinary biomarker sets for specific clinical indications. Currently, physicians order examinations or tests from different disciplines and integrate the data themselves. With ID, clinical questions can be addressed by in vivo and in vitro diagnostic medicine, with different disciplines integrating their respective data and reporting interpreted results to other providers and patients in a combined report. Now is the time for radiologists and pathologists to venture beyond our disciplines and engage the broader diagnostic challenges confronted by ID. In the “Recommendations” section, we provide concrete advice on integration of ID into current practices.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Why ID?
Added clinical value
Good medical practice demands that only clinically appropriate examinations be performed, with minimum achievable risk. Socioeconomics requires that medical examinations be performed in a cost-effective fashion, while minimizing discomfort or inconvenience. The search for value in health care spending often casts imaging and diagnostics as drivers of cost and wasteful overutilization. However, diagnostic examination results are directly or indirectly involved in approximately 70% of medical decision making, while requiring less than 3% of the money spent on health care expenditures. In an effort to ensure value, hospitals, payers, and regulatory agencies track cost and quality performance; ID has the potential to improve both. Predictive analytic tools based on aggregated clinical data can streamline care pathways so that appropriate imaging and diagnostics are prioritized and expedited, on the basis of continual asynchronous informatics tools operating outside of, but in parallel with, direct communications and visits with patient providers.
Our health care delivery system is rife with opportunity for streamlining care and reducing cost. We must find more cost-effective approaches to evaluating and bringing better health care not only to an individual patient but to our populations of patients, especially those who may have been historically disadvantaged. Since 2002, the American Medical Association (AMA) has emphasized the roles and responsibilities of physicians to promote the public’s health.[54] Patients in rural areas often experience barriers to health care, including radiology and laboratory services, that limit their ability to receive appropriate care. Not surprisingly, these deleterious effects are magnified for minority, underserved, and underdeveloped populations.[55] ID offers unique and necessary tools to address these broader social demands on health care.
Local reimbursement systems present formidable barriers to change, including the implementation of ID. The prevailing fee-for-service reimbursement system in the United States offers little incentive to pool intellectual and informatics resources to develop an ID approach. Regulatory constraints around fee sharing have been reduced by the accountable care and bundled payment programs (i.e., the Affordable Care Act), but these programs still represent a minority of health care reimbursement. Even in single-payer systems such as the United Kingdom’s National Health Service, cultural barriers may exist arising from the desire to maintain individual department resources. Importantly, the large capital investments in informatics infrastructure that will be required to manage a robust ID workflow could actually delay innovation when new, more integrated IT systems are needed in the future. The Health Information Technology for Economic and Clinical Health Act of 2009 incentivizing the adoption of EHRs included $27 billion to help finance the endeavor.[56] The current Cures Act does not have comparable governmental financial support. The lack of clarity on how the significant investment required of medical informatics companies will be rewarded represents another reimbursement-related barrier to innovation.
Discovery
Imaging and advanced molecular diagnostics have hastened the pace of discovery by providing quantitative outcome measures and decreasing subject variability in clinical trials, while lessening required sample size.[57] ID can expand our ability to perform efficient clinical trials with diverse patient populations. Using “real-world” data allows pragmatic research based on “computable phenotypes,” resulting in clinical cohorts from multiple sources containing data gathered in clinical care, home, or community settings.[57] It also enables more practical “pseudorandomized” clinical trials, which is important in a setting of decreased margins and demand for faster discovery. Furthermore, many diseases respond to multimodality therapy, and as such, evaluating single therapy interventions using traditional outcome measures and randomized clinical trials may miss therapies with important subclinical effects.
Medical education
ID principles should be formally introduced in the first year of medical school, beginning with the concepts of team medicine and differential diagnosis on the basis of Bayesian inference, and pathologists and radiologists should be active participants. The current organization of undergraduate and graduate medical education fosters departmental silos, compounding fragmented informatics and information infrastructure. Traditional teaching must be changed to reflect the ID workflow, as in the problem-oriented curricula adopted in the Netherlands.[58] Table 2 includes recommendations for ways to encourage ID in medical education.
| ||||||||||||
ID now?
Although separate radiology and pathology departments remain the norm at academic medical centers, early efforts at ID departments have been made. At Erasmus MC, University Medical Center Rotterdam, one of the largest academic hospitals in the Netherlands, clinical departments are organized in themes (G.P. Krestin, personal observation, 2022). The theme "Diagnostics and Advice" gathers all diagnostic departments (radiology and nuclear medicine, pathology, laboratory medicine, microbiology, virology, immunology, and pharmacy). The leadership of the theme consists of the department chairs and is committed to implementing the concept of ID to deliver high-quality ID reports to the referring physicians of the hospital. However, in the initial phase there was resistance from both clinical and diagnostic staff: referring clinicians considered that decision for the choice of diagnostic tests needed to remain their domain, while the diagnostic staff was reluctant to take on board additional “burdensome” exchanges with their colleagues in other diagnostic specialties. To break the deadlock, leadership started with a number of pilot cases (lung cancer, adrenal incidentaloma, primary liver lesions) that all turned out to benefit from an ID approach.
In 2018, the new Dell Medical School of the University of Texas at Austin established the Department of Diagnostic Medicine, which incorporated radiology and pathology (R.N. Bryan, personal observation, 2022). The organization of this department features a tripartite leadership of the chair and co-chairs or chiefs of clinical radiology and pathology. The chair has primary responsibility for the research program, while the clinical chiefs have primary responsibility for their respective clinical services. Responsibility for the educational programs is shared by these three departmental leaders, who are supported by appropriate vice-chairs for education and research from radiology and pathology faculty members. Although still nascent, progress of the program is internally viewed as “encouraging.” Newly Accreditation Council for Graduate Medical Education (ACGME)-credentialed radiology and pathology residency programs will accentuate radiology and pathology teaching conferences and multidisciplinary clinical conferences.
A major limitation to these joint efforts is IT infrastructure. At Erasmus MC, the recent digitization of the pathology department and use of similar image management systems in pathology and radiology is expected to further facilitate integration between these specialties and the health system EHR. At the Dell Medical School, IT remains separate and fragmented, not only between radiology and pathology but also with the hospital EHR and other specialty information systems. Although technological integration of IT infrastructure (RIS, LIS, PACS, EHR, etc.) is necessary for the success of ID, it is not sufficient. Coordinated, multispecialty oversight of the ensemble is critical and must still address the specific needs of each specialty, while at the same time presenting a seamless overview to the clinical, research, and educational communities.
Recommendations
Progress toward a more integrated approach to medical diagnostics has been slow, even in organizations that have created structures to foster it. Silos of expertise and incentives are deeply ingrained. Some might argue that it will take regulation or significant payment innovation to break them down. The digitization of pathology, pathology’s “third revolution,” and the application of AI to medical data create a sense of both possibility and urgency around this effort. Key drivers of success will be organizational matrices that foster communication and collaboration, supported by robust informatics infrastructure. A general model of this concept is the integrated practice unit (IPU), which defines a multidisciplinary team of appropriate clinical and patient support personnel to address the full care cycle of a patient condition, supported by necessary physical, financial, and IT elements.[59] A relatively unique view of the currently ill-defined roles of radiologists and pathologists in an IPU is that of an information specialist.[60] Here, the radiologist’s or pathologist’s responsibility is not just the extraction of information from images or histology but management of that information (plus information extracted by AI) in the clinical context of the patient.
Change must begin with small, easy steps, such as preclinical ID presentations by radiologists and pathologists, more joint radiology and pathology teaching sessions in our graduate medical education programs, focused postgraduate training programs jointly sponsored by our professional organizations, and extension of the tumor board concept into other disciplines, such as heart failure and infectious disease. However, the initial smaller steps should culminate in an organization with the will to implement a strong ID program and a way to support it through robust informatics. Table 2 lists recommendations for changes, some more immediately “doable,” others more demanding but achievable. The previous section described early ID efforts at Erasmus MC and the Dell Medical School. A third example, the Center for Integrated Diagnostics at the Massachusetts General Hospital, with the mission “to foster development of clinical actionable diagnostics and accelerate the adoption of personalized medicine,” also recognizes the need to extend the concept beyond oncology and expand its testing to other disciplines.[61]
The failure of widespread adoption of the IPU concept of disease-focused care does not bode well for the health care system’s ability to adapt.[62] Creating financial models that demonstrate the economic value proposition of ID will be a necessary catalyst for change. We believe creating a clear vision of the value created by ID for patient outcomes and quality of care will be most effective. Berwick’s “dimensions of total quality” are all served by ID: don’t kill me (no needless deaths from improper diagnosis); do help me (with a quick diagnosis); don’t hurt me (no needless pain or unnecessarily invasive tests); don’t make me feel helpless (inform patients of the reason and results of diagnostic tests); don’t keep me waiting (or running between multiple test sites); and don’t waste resources, mine or anyone else’s (perform the fewest, best, least expensive tests).[63]
Abbreviations, acronyms, and initialisms
- ACGME: Accreditation Council for Graduate Medical Education
- AI: artificial intelligence
- AMA: American Medical Association
- CDS: clinical decision support
- EHR: electronic health record
- ID: integrative diagnostics
- IPU: integrated practice unit
- IS: information systems
- IT: information technology
- IS3R: International Society of Strategic Studies in Radiology
- LIS: laboratory information system
- ML: machine learning
- PACS: picture archiving and communication system
- POC: point-of-care
- RIS: radiology information system
- SPOC: single point of contact
Acknowledgements
This paper is published simultaneously in the Journal of the American College of Radiology (DOI: 10.1016/j.jacr.2022.11.015) and Insights into Imaging (DOI: 10.1186/s13244-023-01379-9).
Funding
This work has not received any funding.
Contributions
All authors read and approved the final manuscript.
Competing interest
The authors state that they have no conflict of interest related to the material discussed in this article.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, grammar, and punctuation. In some cases important information was missing from the references, and that information was added. Several URLs were dead in the original; substitute URLs were found for this version. The order of the references in this version differs from the original; the original continues from 40 at Table 2, but this version, by design, lists the references in order of appearance.
- ↑ Saber Tehrani, Ali S; Lee, HeeWon; Mathews, Simon C; Shore, Andrew; Makary, Martin A; Pronovost, Peter J; Newman-Toker, David E (1 August 2013). "25-Year summary of US malpractice claims for diagnostic errors 1986–2010: an analysis from the National Practitioner Data Bank" (in en). BMJ Quality & Safety 22 (8): 672–680. doi:10.1136/bmjqs-2012-001550. ISSN 2044-5415. https://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2012-001550.
- ↑ Graber, Mark L (1 October 2013). "The incidence of diagnostic error in medicine" (in en). BMJ Quality & Safety 22 (Suppl 2): ii21–ii27. doi:10.1136/bmjqs-2012-001615. ISSN 2044-5415. PMC PMC3786666. PMID 23771902. https://qualitysafety.bmj.com/lookup/doi/10.1136/bmjqs-2012-001615.
- ↑ Schwartz, A.; Elstein, A.S. (2019). "Clinical reasoning in medicine". In Higgs, Joy; Jensen, Gail M.; Loftus, Stephen et al.. Clinical reasoning in the health professions (Fourth edition ed.). Edinburgh London New York: Elsevier. pp. 223–234. ISBN 978-0-7020-6224-7.
- ↑ AdvaMedDx (June 2011). "A Policy Primer on Diagnostics". Archived from the original on 01 December 2020. https://web.archive.org/web/20201201141722/https://dx.advamed.org/resource-center?page=4.
- ↑ Van Leeuwen, Anne M.; Bladh, Mickey Lynn (2021). Davis's comprehensive manual of laboratory and diagnostic tests with nursing implications (Ninth edition ed.). Philadelphia: F.A. Davis. ISBN 978-1-7196-4058-9.
- ↑ Lippi, Giuseppe; Plebani, Mario (15 February 2020). "Integrated diagnostics: the future of laboratory medicine?". Biochemia medica 30 (1): 18–30. doi:10.11613/BM.2020.010501. PMC PMC6904966. PMID 31839719. https://www.biochemia-medica.com/en/journal/30/1/10.11613/BM.2020.010501.
- ↑ 7.0 7.1 Committee on Diagnostic Error in Health Care; Board on Health Care Services; Institute of Medicine; The National Academies of Sciences, Engineering, and Medicine (29 December 2015). Balogh, Erin P.; Miller, Bryan T.; Ball, John R.. eds. Improving Diagnosis in Health Care. Washington, D.C.: National Academies Press. doi:10.17226/21794.. ISBN 978-0-309-37769-0. http://www.nap.edu/catalog/21794.
- ↑ Stern, Scott D. C.; Cifu, Adam S.; Altkorn, Diane (2015). Symptom to diagnosis: an evidence-based guide (3rd edition ed.). New York Chicago San Francisco: McGraw-Hill Education Medical. ISBN 978-1-259-25253-2.
- ↑ Lundberg, George D. (2 February 1990). "Critical (Panic) Value Notification: An Established Laboratory Practice Policy (Parameter)" (in en). JAMA: The Journal of the American Medical Association 263 (5): 709. doi:10.1001/jama.1990.03440050103044. ISSN 0098-7484. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.1990.03440050103044.
- ↑ Bleicher, Richard J.; Ruth, Karen; Sigurdson, Elin R.; Beck, J. Robert; Ross, Eric; Wong, Yu-Ning; Patel, Sameer A.; Boraas, Marcia et al. (1 March 2016). "Time to Surgery and Breast Cancer Survival in the United States" (in en). JAMA Oncology 2 (3): 330. doi:10.1001/jamaoncol.2015.4508. ISSN 2374-2437. PMC PMC4788555. PMID 26659430. http://oncology.jamanetwork.com/article.aspx?doi=10.1001/jamaoncol.2015.4508.
- ↑ Zhi, Ming; Ding, Eric L.; Theisen-Toupal, Jesse; Whelan, Julia; Arnaout, Ramy (15 November 2013). Szecsi, Pal Bela. ed. "The Landscape of Inappropriate Laboratory Testing: A 15-Year Meta-Analysis" (in en). PLoS ONE 8 (11): e78962. doi:10.1371/journal.pone.0078962. ISSN 1932-6203. PMC PMC3829815. PMID 24260139. https://dx.plos.org/10.1371/journal.pone.0078962.
- ↑ Hughes, Danny R.; Jiang, Miao; Duszak, Richard (1 January 2015). "A Comparison of Diagnostic Imaging Ordering Patterns Between Advanced Practice Clinicians and Primary Care Physicians Following Office-Based Evaluation and Management Visits" (in en). JAMA Internal Medicine 175 (1): 101. doi:10.1001/jamainternmed.2014.6349. ISSN 2168-6106. http://archinte.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2014.6349.
- ↑ Berner, E.S. (June 2009). "Clinical decision support systems: State of the Art" (PDF). Agency for Healthcare Research and Quality. https://digital.ahrq.gov/sites/default/files/docs/page/09-0069-EF_1.pdf.
- ↑ Blackmore, C. Craig; Mecklenburg, Robert S.; Kaplan, Gary S. (1 January 2011). "Effectiveness of Clinical Decision Support in Controlling Inappropriate Imaging" (in en). Journal of the American College of Radiology 8 (1): 19–25. doi:10.1016/j.jacr.2010.07.009. https://linkinghub.elsevier.com/retrieve/pii/S1546144010003893.
- ↑ Were, M. C.; Shen, C.; Tierney, W. M.; Mamlin, J. J.; Biondich, P. G.; Li, X.; Kimaiyo, S.; Mamlin, B. W. (1 March 2011). "Evaluation of computer-generated reminders to improve CD4 laboratory monitoring in sub-Saharan Africa: a prospective comparative study" (in en). Journal of the American Medical Informatics Association 18 (2): 150–155. doi:10.1136/jamia.2010.005520. ISSN 1067-5027. PMC PMC3116261. PMID 21252053. https://academic.oup.com/jamia/article-lookup/doi/10.1136/jamia.2010.005520.
- ↑ Lacy, N. L. (1 November 2004). "Why We Don't Come: Patient Perceptions on No-Shows" (in en). The Annals of Family Medicine 2 (6): 541–545. doi:10.1370/afm.123. ISSN 1544-1709. PMC PMC1466756. PMID 15576538. http://www.annfammed.org/cgi/doi/10.1370/afm.123.
- ↑ AdvaMedDx (14 November 2019). "From Test To Treatment: The Value Of Diagnostics". https://dx.advamed.org/member-center/resource-library/from-test-to-treatment-the-value-of-diagnostics/. Retrieved 25 February 2022.
- ↑ Ebinger, Martin; Siegerink, Bob; Kunz, Alexander; Wendt, Matthias; Weber, Joachim E.; Schwabauer, Eugen; Geisler, Frederik; Freitag, Erik et al. (2 February 2021). "Association Between Dispatch of Mobile Stroke Units and Functional Outcomes Among Patients With Acute Ischemic Stroke in Berlin" (in en). JAMA 325 (5): 454. doi:10.1001/jama.2020.26345. ISSN 0098-7484. PMC PMC7856548. PMID 33528537. https://jamanetwork.com/journals/jama/fullarticle/2775714.
- ↑ Lu, Michael T.; Rosman, David A.; Wu, Carol C.; Gilman, Matthew D.; Harvey, H. Benjamin; Gervais, Debra A.; Alkasab, Tarik K.; Shepard, Jo-Anne O. et al. (1 February 2016). "Radiologist Point-of-Care Clinical Decision Support and Adherence to Guidelines for Incidental Lung Nodules" (in en). Journal of the American College of Radiology 13 (2): 156–162. doi:10.1016/j.jacr.2015.09.029. https://linkinghub.elsevier.com/retrieve/pii/S1546144015009667.
- ↑ Zwaan, Laura; Thijs, Abel; Wagner, Cordula; Timmermans, Daniëlle R.M. (1 August 2013). "Does inappropriate selectivity in information use relate to diagnostic errors and patient harm? The diagnosis of patients with dyspnea" (in en). Social Science & Medicine 91: 32–38. doi:10.1016/j.socscimed.2013.05.001. https://linkinghub.elsevier.com/retrieve/pii/S0277953613002682.
- ↑ Wahls, Terry L; Cram, Peter M (1 December 2007). "The frequency of missed test results and associated treatment delays in a highly computerized health system" (in en). BMC Family Practice 8 (1): 32. doi:10.1186/1471-2296-8-32. ISSN 1471-2296. PMC PMC1891295. PMID 17519017. https://bmcfampract.biomedcentral.com/articles/10.1186/1471-2296-8-32.
- ↑ Allyn, J. (29 August 2019). "RSNA/AAPM Symposium Addresses Integrated Diagnostics at RSNA 2019". Radiological Society of North America. https://www.rsna.org/news/2019/August/Integrated-Diagnostics.
- ↑ Harmony Healthcare IT (4 August 2020). "Health Data Volumes Skyrocket, Legacy Data Archives On the Rise". https://www.harmonyhit.com/health-data-volumes-skyrocket-legacy-data-archives-rise-hie/. Retrieved 15 November 2021.
- ↑ RBC Capital Markets (2021). "The Healthcare Data Explosion". RBC Dominion Securities Inc. https://www.rbccm.com/en/gib/healthcare/episode/the_healthcare_data_explosion#content-panel. Retrieved 15 November 2021.
- ↑ Association of State and Territorial Health Officials (2016). "Public Health Informatics". Medicaid and Public Health Integration Learning Series. Archived from the original on 08 November 2019. https://web.archive.org/web/20191108083841/http://www.astho.org/Health-Systems-Transformation/Medicaid-and-Public-Health-Partnerships/Learning-Series/Public-Health-Informatics/.
- ↑ Riches, Nicholas; Panagioti, Maria; Alam, Rahul; Cheraghi-Sohi, Sudeh; Campbell, Stephen; Esmail, Aneez; Bower, Peter (8 March 2016). Schmidt, Robert L. ed. "The Effectiveness of Electronic Differential Diagnoses (DDX) Generators: A Systematic Review and Meta-Analysis" (in en). PLOS ONE 11 (3): e0148991. doi:10.1371/journal.pone.0148991. ISSN 1932-6203. PMC PMC4782994. PMID 26954234. https://dx.plos.org/10.1371/journal.pone.0148991.
- ↑ "21st Century Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program - 85 FR 25642". Federal Register. U.S. Government Publishing Office. 1 May 2020. https://www.federalregister.gov/documents/2020/05/01/2020-07419/21st-century-cures-act-interoperability-information-blocking-and-the-onc-health-it-certification.
- ↑ "ESR reaches out to Clinical Chemistry and Laboratory Medicine". European Society of Radiology. September 2019. http://www.myesr.link/Mailings/esr@work-september-2019/. Retrieved 26 May 2022.
- ↑ Pelsers, Maurice M A L; Hanhoff, Thorsten; Van der Voort, Daniëlle; Arts, Baer; Peters, Maarten; Ponds, Rudolf; Honig, Adriaan; Rudzinski, Wojtek et al. (1 September 2004). "Brain- and Heart-Type Fatty Acid-Binding Proteins in the Brain: Tissue Distribution and Clinical Utility" (in en). Clinical Chemistry 50 (9): 1568–1575. doi:10.1373/clinchem.2003.030361. ISSN 0009-9147. https://academic.oup.com/clinchem/article/50/9/1568/5640128.
- ↑ Ponti, Giovanni; Maccaferri, Monia; Percesepe, Antonio; Tomasi, Aldo; Ozben, Tomris (2 January 2021). "Liquid biopsy with cell free DNA: new horizons for prostate cancer" (in en). Critical Reviews in Clinical Laboratory Sciences 58 (1): 60–76. doi:10.1080/10408363.2020.1803789. ISSN 1040-8363. https://www.tandfonline.com/doi/full/10.1080/10408363.2020.1803789.
- ↑ Gao, Yanyun; Zhang, Meng; Li, Xiulian; Zeng, Pengjiao; Wang, Peitao; Zhang, Lijuan (2019), "Serum PSA levels in patients with prostate cancer and other 33 different types of diseases" (in en), Progress in Molecular Biology and Translational Science (Elsevier) 162: 377–390, doi:10.1016/bs.pmbts.2018.12.013, ISBN 978-0-12-817738-9, https://linkinghub.elsevier.com/retrieve/pii/S1877117318301613. Retrieved 2023-04-04
- ↑ Bhalla, Amarpreet; Zulfiqar, Muhammad; Bluth, Martin H. (1 June 2018). "Molecular Diagnostics in Colorectal Carcinoma" (in en). Clinics in Laboratory Medicine 38 (2): 311–342. doi:10.1016/j.cll.2018.02.008. https://linkinghub.elsevier.com/retrieve/pii/S0272271218300088.
- ↑ Delgado, Jose Antonio; Ballesteros, Maria Antonieta; Parera, María Magdalena; Bauça, Josep Miquel (2 November 2021). "Pancreatic Cancer Insights: Optimization of the Diagnostic Capacity of Tumor Biomarkers" (in en). Laboratory Medicine 52 (6): 550–557. doi:10.1093/labmed/lmab016. ISSN 0007-5027. https://academic.oup.com/labmed/article/52/6/550/6253743.
- ↑ Li, Xiulian; Xu, Yan; Zhang, Lijuan (2019), "Serum CA153 as biomarker for cancer and noncancer diseases" (in en), Progress in Molecular Biology and Translational Science (Elsevier) 162: 265–276, doi:10.1016/bs.pmbts.2019.01.005, ISBN 978-0-12-817738-9, https://linkinghub.elsevier.com/retrieve/pii/S187711731930016X. Retrieved 2023-04-04
- ↑ Heizmann, Claus W. (1 July 2019). "S100 proteins: Diagnostic and prognostic biomarkers in laboratory medicine" (in en). Biochimica et Biophysica Acta (BBA) - Molecular Cell Research 1866 (7): 1197–1206. doi:10.1016/j.bbamcr.2018.10.015. https://linkinghub.elsevier.com/retrieve/pii/S0167488918304786.
- ↑ Wang, Hongchun; Zhang, Jian; Li, Xiaoli; Zhang, Cheng; Zheng, Shuli; Chi, Yihong; Sheng, Xia; Zhang, Yi (1 November 2020). "The utilization pattern of serum tumor markers in lung cancer patients: A population‐based retrospective descriptive study" (in en). Journal of Clinical Laboratory Analysis 34 (11). doi:10.1002/jcla.23465. ISSN 0887-8013. PMC PMC7676212. PMID 32638440. https://onlinelibrary.wiley.com/doi/10.1002/jcla.23465.
- ↑ Milani, Paolo; Palladini, Giovanni; Merlini, Giampaolo (13 July 2016). "Serum-free light-chain analysis in diagnosis and management of multiple myeloma and related conditions" (in en). Scandinavian Journal of Clinical and Laboratory Investigation 76 (sup245): S113–S118. doi:10.1080/00365513.2016.1210337. ISSN 0036-5513. https://www.tandfonline.com/doi/full/10.1080/00365513.2016.1210337.
- ↑ Shi, Min; Xiao, Ruobing; Woda, Bruce A.; Yu, Hongbo (1 March 2014). "Five Important Advances in Hematopathology" (in en). Archives of Pathology & Laboratory Medicine 138 (3): 410–419. doi:10.5858/ARPA.2012-0645-RA. ISSN 1543-2165. http://meridian.allenpress.com/aplm/article/138/3/410/132807/Five-Important-Advances-in-Hematopathology.
- ↑ Jacob, Rachel; Khan, Mahmood (1 December 2018). "Cardiac Biomarkers: What Is and What Can Be" (in en). Indian Journal of Cardiovascular Disease in Women WINCARS 03 (04): 240–244. doi:10.1055/s-0039-1679104. ISSN 2455-7854. PMC PMC6957084. PMID 31934672. http://www.thieme-connect.de/DOI/DOI?10.1055/s-0039-1679104.
- ↑ Ferry, Olivia R.; Huang, Yao C.; Masel, Philip J.; Hamilton, Michael; Fong, Kwun M.; Bowman, Rayleen V.; McKenzie, Scott C.; Yang, Ian A. (1 October 2019). "Diagnostic approach to chronic dyspnoea in adults". Journal of Thoracic Disease 11 (S17): S2117–S2128. doi:10.21037/jtd.2019.10.53. PMC PMC6831921. PMID 31737340. http://jtd.amegroups.com/article/view/32611/22932.
- ↑ Dagonnier, Marie; Donnan, Geoffrey A.; Davis, Stephen M.; Dewey, Helen M.; Howells, David W. (5 February 2021). "Acute Stroke Biomarkers: Are We There Yet?". Frontiers in Neurology 12: 619721. doi:10.3389/fneur.2021.619721. ISSN 1664-2295. PMC PMC7902038. PMID 33633673. https://www.frontiersin.org/articles/10.3389/fneur.2021.619721/full.
- ↑ Wall, Emma C.; Chan, Jia Mun; Gil, Eliza; Heyderman, Robert S. (1 June 2021). "Acute bacterial meningitis" (in en). Current Opinion in Neurology 34 (3): 386–395. doi:10.1097/WCO.0000000000000934. ISSN 1350-7540. PMC PMC7610733. PMID 33767093. https://journals.lww.com/10.1097/WCO.0000000000000934.
- ↑ Goldsmith, Joshua F.; Herskovits, A. Zara (1 September 2020). "Cerebrospinal Fluid Testing for Multiple Sclerosis" (in en). Clinics in Laboratory Medicine 40 (3): 369–377. doi:10.1016/j.cll.2020.06.002. https://linkinghub.elsevier.com/retrieve/pii/S027227122030041X.
- ↑ Schuurman, Alex R.; Reijnders, Tom D. Y.; Kullberg, Robert F. J.; Butler, Joe M.; van der Poll, Tom; Wiersinga, W. Joost (1 December 2021). "Sepsis: deriving biological meaning and clinical applications from high-dimensional data" (in en). Intensive Care Medicine Experimental 9 (1): 27. doi:10.1186/s40635-021-00383-x. ISSN 2197-425X. PMC PMC8105470. PMID 33961170. https://icm-experimental.springeropen.com/articles/10.1186/s40635-021-00383-x.
- ↑ Espinoza, Gianna; Maldonado, Genessis; Narvaez, Jemina; Guerrero, Roberto; Citera, Gustavo; Rios, Carlos (1 March 2021). "Beyond Rheumatoid Arthritis Evaluation: What are We Missing?" (in en). Open Access Rheumatology: Research and Reviews Volume 13: 45–55. doi:10.2147/OARRR.S298393. ISSN 1179-156X. PMC PMC8007602. PMID 33790666. https://www.dovepress.com/beyond-rheumatoid-arthritis-evaluation-what-are-we-missing-peer-reviewed-article-OARRR.
- ↑ Petrovská, Nora; Prajzlerová, Klára; Vencovský, Jiří; Šenolt, Ladislav; Filková, Mária (1 May 2021). "The pre-clinical phase of rheumatoid arthritis: From risk factors to prevention of arthritis" (in en). Autoimmunity Reviews 20 (5): 102797. doi:10.1016/j.autrev.2021.102797. https://linkinghub.elsevier.com/retrieve/pii/S1568997221000616.
- ↑ Betterle, C.; Presotto, F.; Furmaniak, J. (1 December 2019). "Epidemiology, pathogenesis, and diagnosis of Addison’s disease in adults" (in en). Journal of Endocrinological Investigation 42 (12): 1407–1433. doi:10.1007/s40618-019-01079-6. ISSN 1720-8386. https://link.springer.com/10.1007/s40618-019-01079-6.
- ↑ Stavropoulos, Konstantinos; Imprialos, Konstantinos; Papademetriou, Vasilios; Faselis, Charles; Tsioufis, Kostas; Dimitriadis, Kyriakos; Doumas, Michael (2020). "Primary Aldosteronism: Novel Insights". Current Hypertension Reviews 16 (1): 19–23. doi:10.2174/1573402115666190415155512. ISSN 1875-6506. PMID 30987572. https://pubmed.ncbi.nlm.nih.gov/30987572.
- ↑ Honegger, Jürgen; Buchfelder, Michael; Schlaffer, Sven; Droste, Michael; Werner, Sandy; Strasburger, Christian; Störmann, Sylvère; Schopohl, Jochen et al. (1 September 2015). "Treatment of Primary Hypophysitis in Germany" (in en). The Journal of Clinical Endocrinology & Metabolism 100 (9): 3460–3469. doi:10.1210/jc.2015-2146. ISSN 0021-972X. https://academic.oup.com/jcem/article-lookup/doi/10.1210/jc.2015-2146.
- ↑ Serbis, Anastasios; Giapros, Vasileios; Kotanidou, Eleni P; Galli-Tsinopoulou, Assimina; Siomou, Ekaterini (15 April 2021). "Diagnosis, treatment and prevention of type 2 diabetes mellitus in children and adolescents". World Journal of Diabetes 12 (4): 344–365. doi:10.4239/wjd.v12.i4.344. ISSN 1948-9358. PMC PMC8040084. PMID 33889284. https://www.wjgnet.com/1948-9358/full/v12/i4/344.htm.
- ↑ Supabphol, Suangson; Seubwai, Wunchana; Wongkham, Sopit; Saengboonmee, Charupong (1 September 2021). "High glucose: an emerging association between diabetes mellitus and cancer progression" (in en). Journal of Molecular Medicine 99 (9): 1175–1193. doi:10.1007/s00109-021-02096-w. ISSN 0946-2716. https://link.springer.com/10.1007/s00109-021-02096-w.
- ↑ LeGrys, Vicky A.; Hartmann, Katherine; Walsh, Joan F. (2004). "The clinical consequences and diagnosis of hypothyroidism". Clinical Laboratory Science: Journal of the American Society for Medical Technology 17 (4): 203–208. ISSN 0894-959X. PMID 15559725. https://pubmed.ncbi.nlm.nih.gov/15559725.
- ↑ Pignatelli, Duarte; Carvalho, Berta L.; Palmeiro, Aida; Barros, Alberto; Guerreiro, Susana G.; Macut, Djuro (4 July 2019). "The Complexities in Genotyping of Congenital Adrenal Hyperplasia: 21-Hydroxylase Deficiency". Frontiers in Endocrinology 10: 432. doi:10.3389/fendo.2019.00432. ISSN 1664-2392. PMC PMC6620563. PMID 31333583. https://www.frontiersin.org/article/10.3389/fendo.2019.00432/full.
- ↑ Elster, A (1 April 2002). "Physician roles in medicine-public health collaboration future directions of the American Medical Association". American Journal of Preventive Medicine 22 (3): 211–213. doi:10.1016/S0749-3797(01)00422-6. https://linkinghub.elsevier.com/retrieve/pii/S0749379701004226.
- ↑ Emerson, Marc A.; Golightly, Yvonne M.; Aiello, Allison E.; Reeder‐Hayes, Katherine E.; Tan, Xianming; Maduekwe, Ugwuji; Johnson‐Thompson, Marian; Olshan, Andrew F. et al. (15 November 2020). "Breast cancer treatment delays by socioeconomic and health care access latent classes in Black and White women" (in en). Cancer 126 (22): 4957–4966. doi:10.1002/cncr.33121. ISSN 0008-543X. PMC PMC7789230. PMID 32954493. https://onlinelibrary.wiley.com/doi/10.1002/cncr.33121.
- ↑ Schilling, B. (2011). "The Federal Government Has Put Billions into Promoting Electronic Health Record Use: How Is It Going?". The Commonwealth Fund. https://www.commonwealthfund.org/publications/newsletter-article/federal-government-has-put-billions-promoting-electronic-health. Retrieved 26 August 2022.
- ↑ 57.0 57.1 Sherman, Rachel E.; Anderson, Steven A.; Dal Pan, Gerald J.; Gray, Gerry W.; Gross, Thomas; Hunter, Nina L.; LaVange, Lisa; Marinac-Dabic, Danica et al. (8 December 2016). "Real-World Evidence — What Is It and What Can It Tell Us?" (in en). New England Journal of Medicine 375 (23): 2293–2297. doi:10.1056/NEJMsb1609216. ISSN 0028-4793. http://www.nejm.org/doi/10.1056/NEJMsb1609216.
- ↑ Bate, Emily; Hommes, Juliette; Duvivier, Robbert; Taylor, David C. M. (1 January 2014). "Problem-based learning (PBL): Getting the most out of your students – Their roles and responsibilities: AMEE Guide No. 84" (in en). Medical Teacher 36 (1): 1–12. doi:10.3109/0142159X.2014.848269. ISSN 0142-159X. http://www.tandfonline.com/doi/full/10.3109/0142159X.2014.848269.
- ↑ Porter, Michael E.; Lee, Thomas H. (1 January 2021). "Integrated Practice Units: A Playbook for Health Care Leaders" (in en). NEJM Catalyst 2 (1): CAT.20.0237. doi:10.1056/CAT.20.0237. ISSN 2642-0007. http://catalyst.nejm.org/doi/10.1056/CAT.20.0237.
- ↑ Jha, Saurabh; Topol, Eric J. (13 December 2016). "Adapting to Artificial Intelligence: Radiologists and Pathologists as Information Specialists" (in en). JAMA 316 (22): 2353. doi:10.1001/jama.2016.17438. ISSN 0098-7484. http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.2016.17438.
- ↑ "Department of Pathology, Center for Integrated Diagnostics". Massachusetts General Hospital. https://www.massgeneral.org/pathology/services/center-for-integrated-diagnostics. Retrieved 15 November 2021.
- ↑ Eickholt, Lynne (1 January 2020). "Why Many Integrated Delivery Systems Have Not Enhanced Consumer Value, and What’s Next" (in en). NEJM Catalyst 1 (1): CAT.19.1086. doi:10.1056/CAT.19.1086. ISSN 2642-0007. http://catalyst.nejm.org/doi/10.1056/CAT.19.1086.
- ↑ Berwick, Donald M. (18 January 2005). "My Right Knee" (in en). Annals of Internal Medicine 142 (2): 121-5. doi:10.7326/0003-4819-142-2-200501180-00011. ISSN 0003-4819. http://annals.org/article.aspx?doi=10.7326/0003-4819-142-2-200501180-00011.